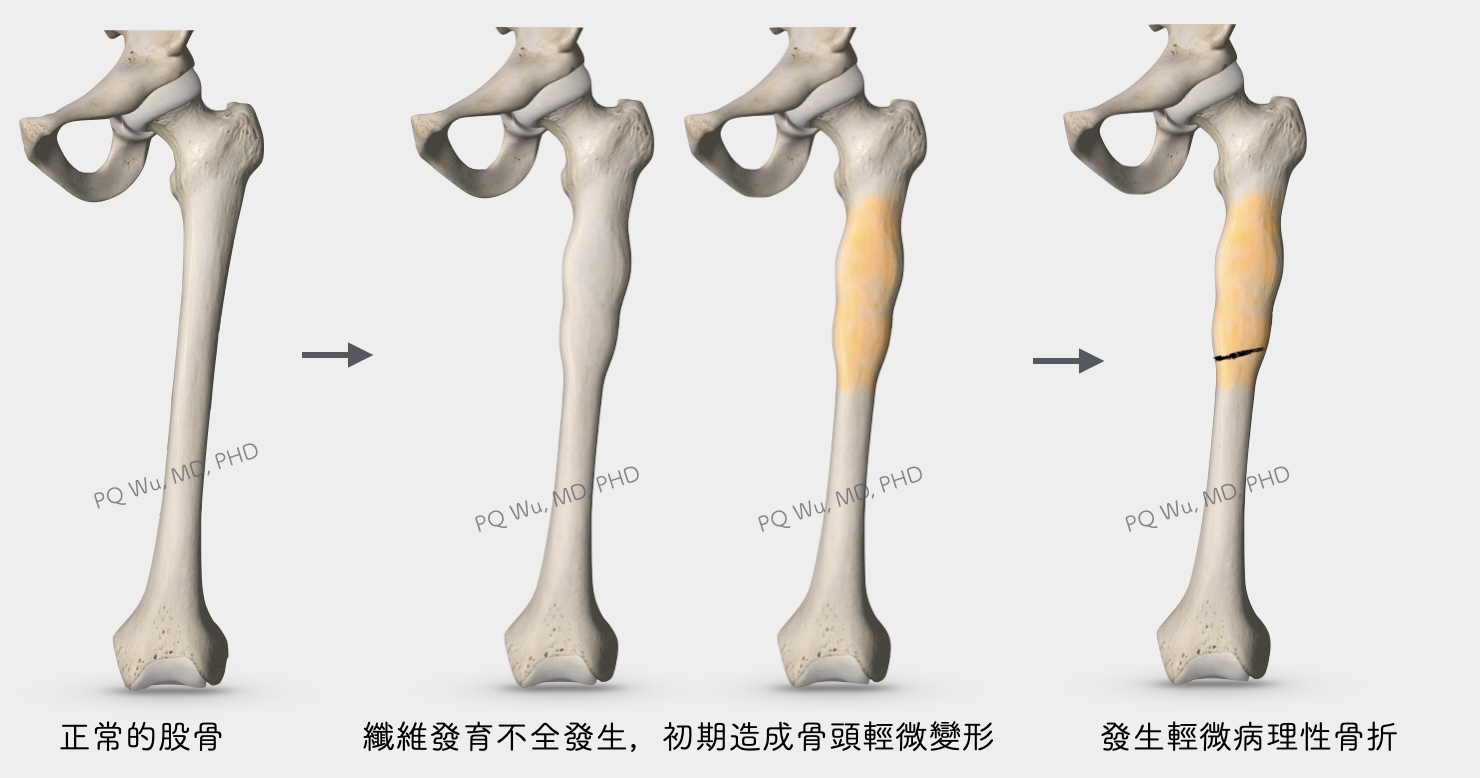
Fibrous dysplasia is a relatively common tumor that is mostly found in adults. The main problem with tumors is that normal bones are replaced by abnormal fibrous tissues and immature bone tissues, causing a softer bone structure. Fibrous dysplasia is mostly accidentally found, and unless the tumor becomes large, most would need only regular tracking, not a surgical treatment.
Chinese: None
English: fibrous osteodystrophy, osteodystrophia fibrosa, and osteitis fibrosa disseminate
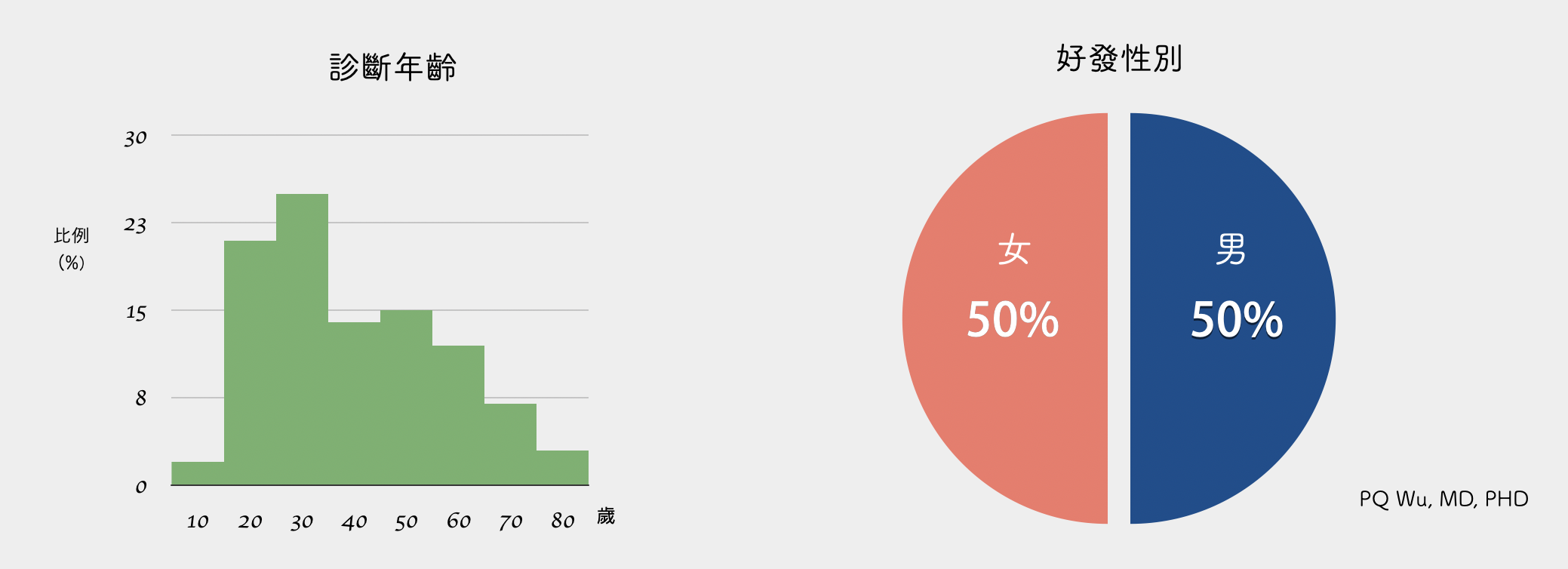
Most patients with fibrous dysplasia are mostly asymptomatic and may experience a little discomfort at the lesion during more intense exercise. Most tumors are found by chance after a physical examination or by an X-ray diagnosis of other problems. The age of discovery is between 20 and 30 years old. However, if the tumor grows in the body area that carries more weight, such as the region near the hip joint, the patient may experience pain during exercise and go to a doctor.
Or, in a few cases, when the region of tumor invasion is relatively wide, it will cause local swelling and deformation at the lesion, and more serious, even pathogenic fractures will incur.
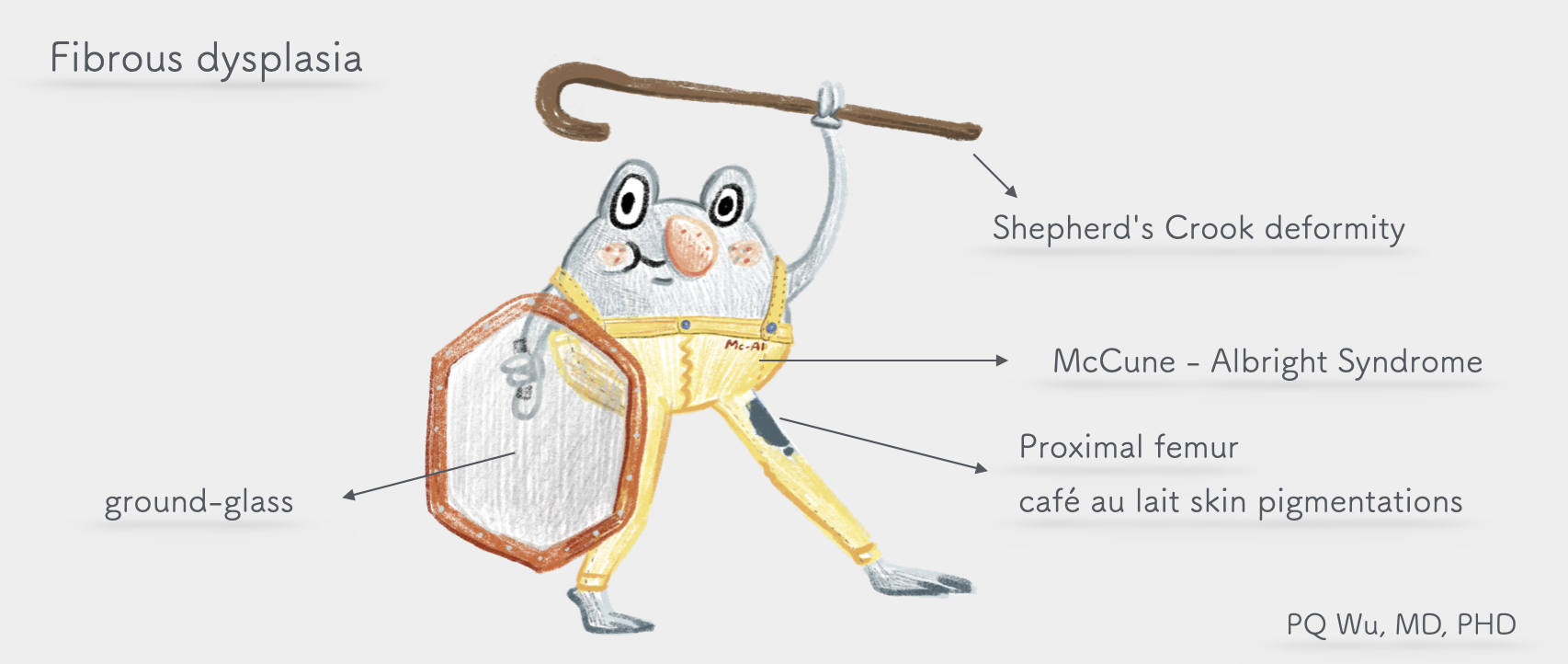
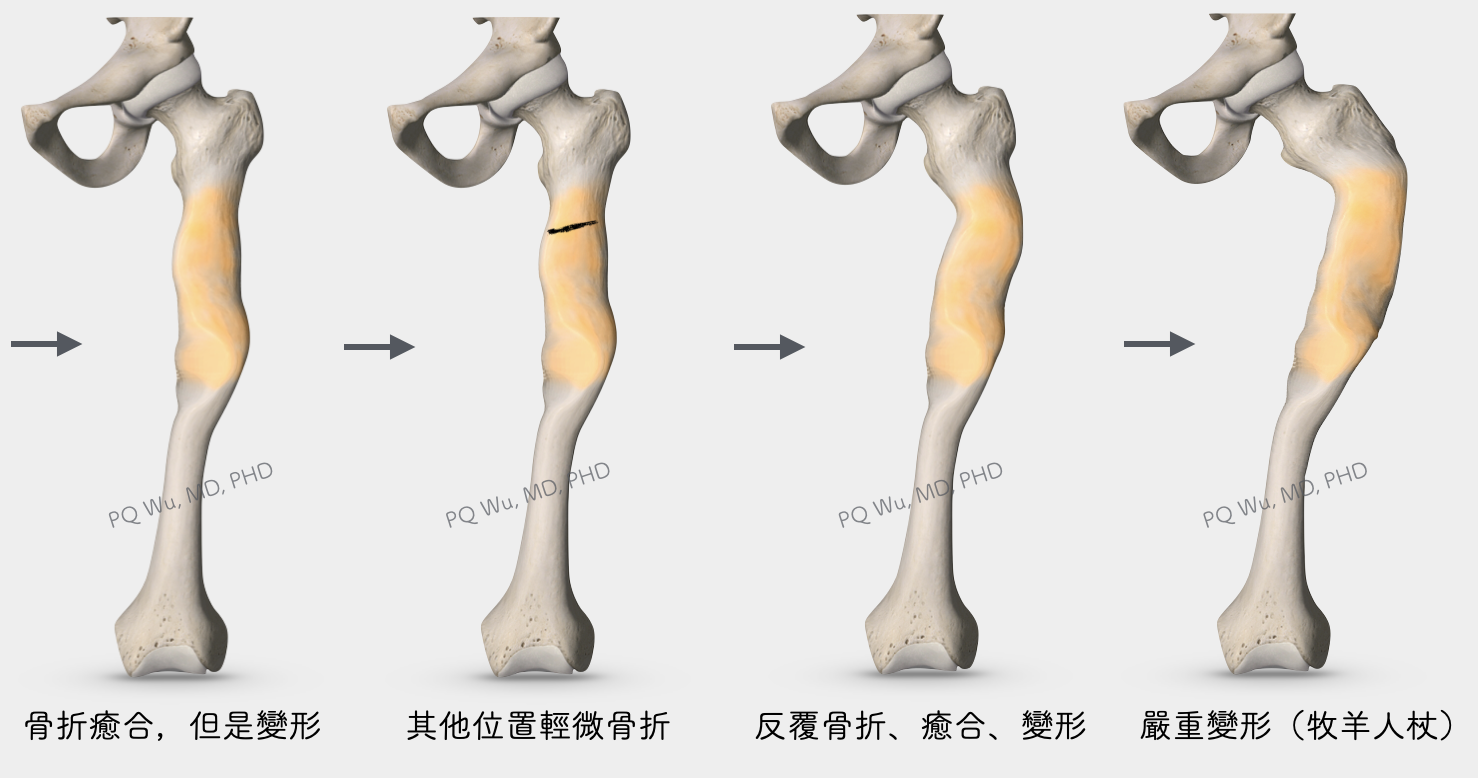
Fractures in fibrous dysplasia, compared to other tumors, have a different characteristic. Because the invaded bone has softer composition, the fractures usually do not break the whole bone but are partial, linked like broken wire or chopsticks. The patient may then feel pain for a few weeks before it alleviates gradually. However, the fractured part would deform because of weight-bearing. After many times of fractures, healings, and deformations, the patient's feet would slowly become curved, like a shepherd's crutch, which is medically known as the 'Shepherd's Crook deformity'.
Fibrous dysplasia is a common benign bone tumor. Since most of the cases are asymptomatic and stay steady with patients, medical diagnoses are usually not seeking, and the correct incidence cannot be estimated. However, rough estimation is about 7% of benign bone tumors. Our outpatient clinic would discover approximately 10 to 15 new patients in about one month at the Therapeutical and Research Center of Musculoskeletal Tumor in Taipei Veterans General Hospital.
Fibrous dysplasia has a similar occurrence rate between men to women. Most of the cases occur in adults between the ages of 20 and 40.
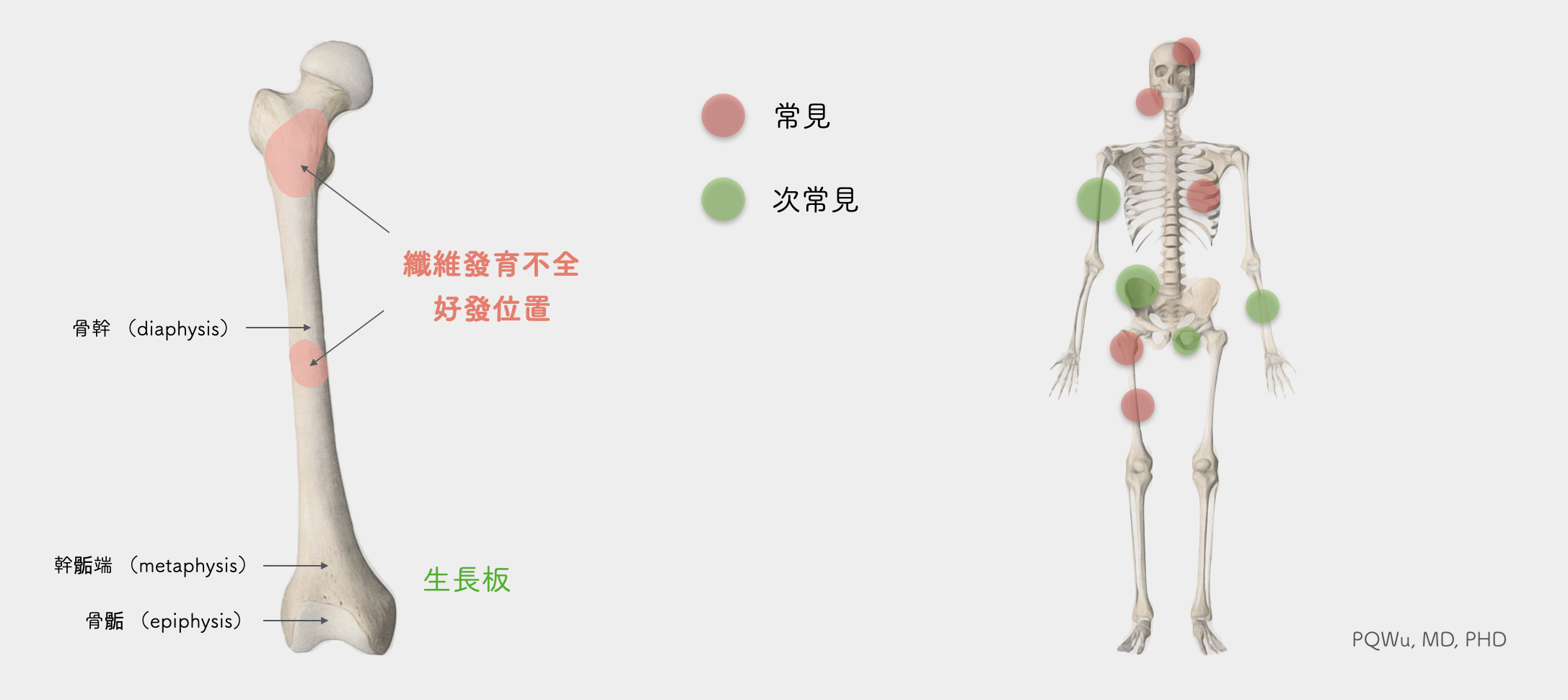
Fibrous dysplasia can occur in many bones, and the most likely locations are the proximal femur, tibia, rib, and skull. Fibrous dysplasias that grow in the ribs or skulls are usually asymptomatic. If it grows in the proximal femur, the patient would feel asthenic that during regular activity or, in the worst case, suffer pain and minor fractures and deformations because it is the bone that bears weights.
Most fibrous dysplasias grow from the center of the bone, which locates mostly at metaphysis and diaphysis, and less invasive to the epiphysis and joint surface. Medically, we divide the bones into epiphysis, metaphysis, and diaphysis. Most bone tumors occur at the epiphysis
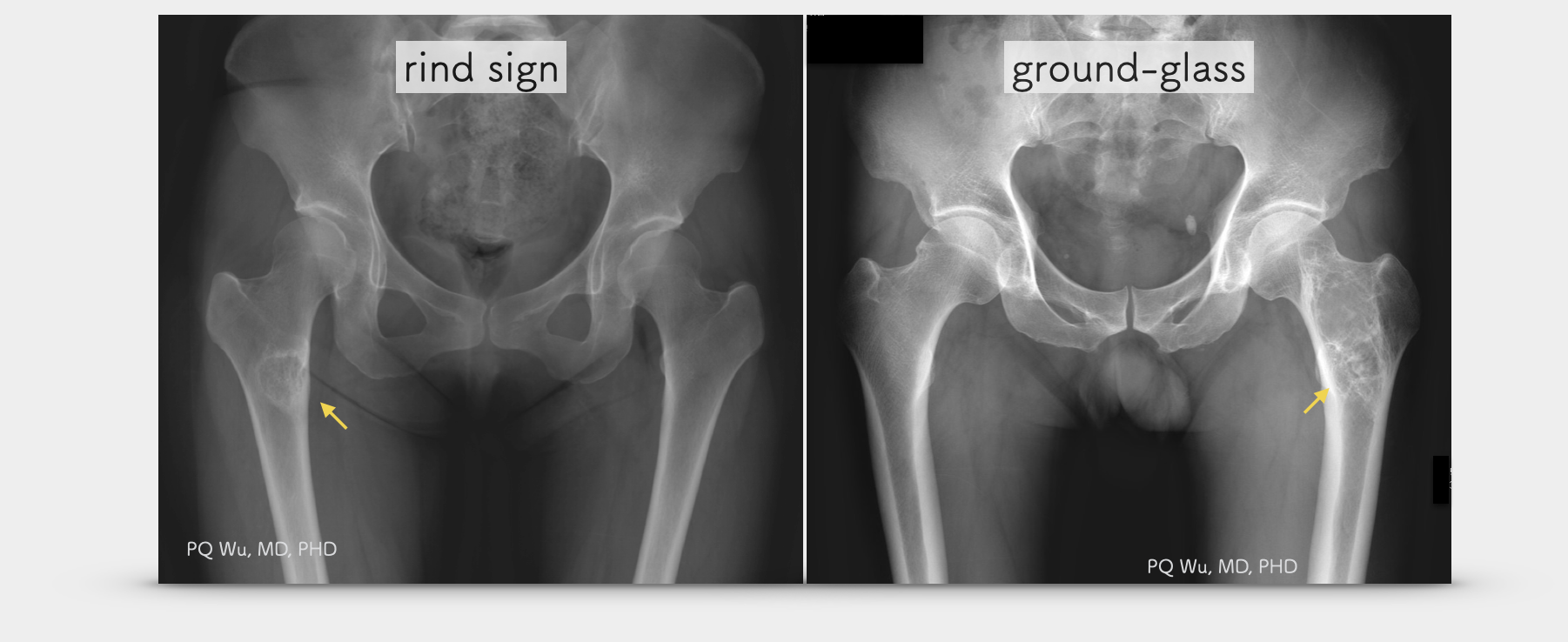
Fibrous dysplasia is caused by the proliferation of abnormal fibrous tissue and osseous tissue. Therefore, its expression under the X-ray is related to the proportion of these fibrous tissues to osseous tissue. It will show higher radiolucency if there are more fibrous tissues, which produce what we call ground-glass phenomena. Conversely, if there is more osseous tissue, it will show higher bone sclerosis, or a circle of hardened bone shell, or rind signs, will appear around the tumor.
The MRI expression of fibrous dysplasia is inconsistent. Sometimes it will have the same expression as that of a general tumor, with a low T1 signal and a high T2 signal, yet sometimes it expresses both low T1 and T2 signals. In general, however, MRI is not necessary for fibrous dysplasia diagnosis since the X-ray expression of fibrous dysplasia is quite unique. Hence, experienced physicians could diagnose it without an MRI image.
When it comes to the causes of fibrous dysplasia, it goes to an important study report published in Genetics in 1992 by Dr. Schwindinger, Dr. Francomano, and Dr. Levine at Johns Hopkins University. The study analyzed the genome of a 53-year-old patient with multiple fibrous dysplasias. They found that one of the patient's G protein controlling gene mutated, resulting in the enhancement of adenyl cyclase activity, and generated subsequent bone, skin pigmentation, and endocrine problems. The gene was later named the GNAS1 gene. The current scientific evidence suggests that the mutation in this gene is postzygotic. (Namely, the mutation is caused by ourselves, not inherited from our parents, nor will it pass to the next generation!)
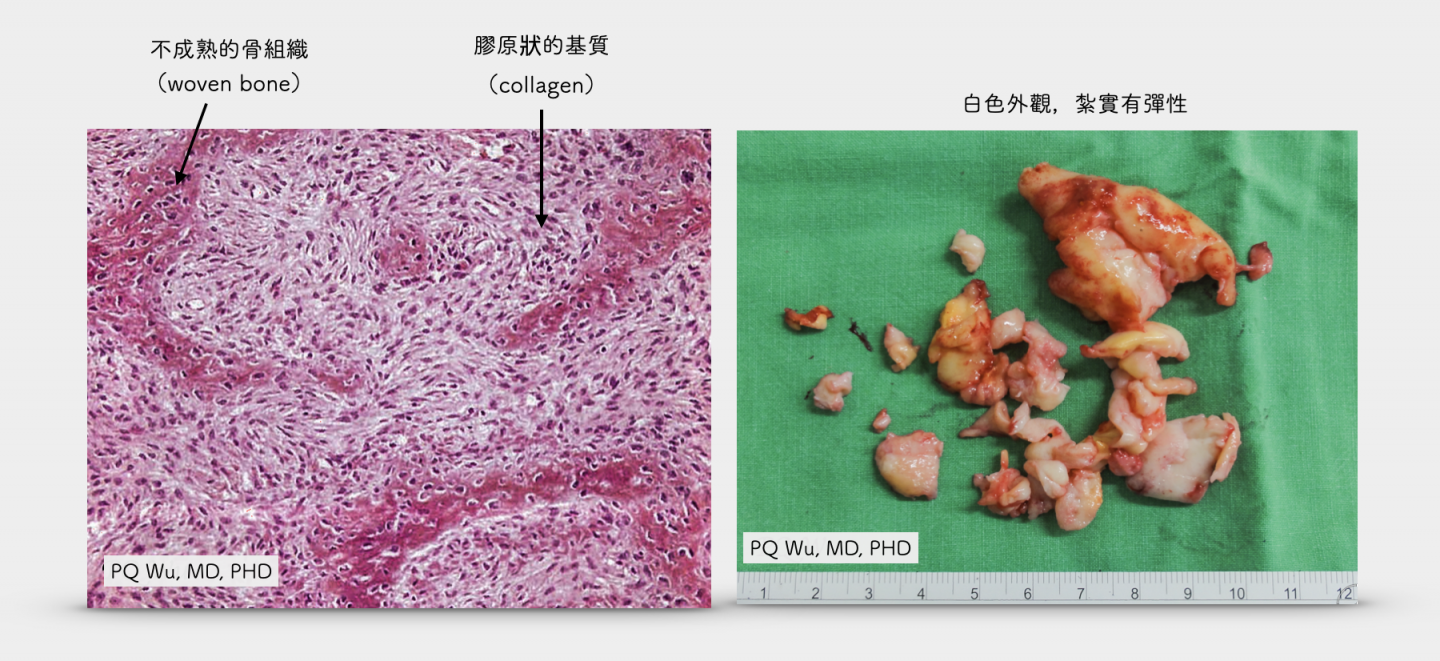
Fibrous dysplasia looks like a scallop, which is relatively solid and elastic. Microscopic observations show that many fibroblasts produce a massive collagen matrix. In the collagen matrix, many immature bone tissues, or woven bone, distribute irregularly. Since the osseous tissues are not as normal as our general tissues, which are arranged regularly and have normal ossification ability, so they do not provide sufficient weight-bearing capability. Therefore, a pathological fracture will occur if the tumor is large because the bone is 'softer'.
About a quarter of fibrous dysplasia is multiple
by PQ Wu
About 20-30% of fibrous dysplasias are multiple. If multiple fibrous dysplasias combines with other internal medicine diseases, we call it McCune-Albright Syndrome. It is named after the pediatrician, Dr. Donovan McCune, and the endocrinologist, Dr. Fuller Albright, at the Johns Hopkins Hospital in 1937.
They found that patients had three common symptoms- The first is skin pigmentation, the second is the abnormal bone structure, and the third is abnormal endocrine secretions. The incidence of McCune-Albright Syndrome is not high and is generally estimated to be between one in 100,000 and one in a million.
The current definition of McCune-Albright Syndrome is that the patient will meet the following classic triad:
1. Polyostotic fibrous dysplasia
2. Cafe au lait skin pigmentation
3. Hyperfunction in the endocrine system, including precocious puberty or other problems such as the pituitary gland, adrenal gland, or thyroid gland issues.
We can also choose genetic testing to identify whether a GNAS1 mutation exists for the diagnosis. However, since it's generally costly and provides the less clinical significance, it is not a routine examination. As mentioned earlier, fibrous dysplasia is a postzygotic mutation; so, if the mutated cells appear early in embryonic development, the cells will have wider distribution, resulting in greater effects to the individual afterward.
This is why fibrous dysplasia is consistent among patients, which expresses from almost completely asymptomatic to pathological fractures and even to endocrine dysfunction. But even the patients with more serious McCune-Albright syndrome have substantial prognoses. Although currently, we don't have a cure for it, we can control other physical problems via proper medication.
Fibrous dysplasia is almost not possible to turn malignant
by PQ Wu
Pure fibrous dysplasia has less than 1% of the likelihood of turning malignant, but in patients with multiple fibrous dysplasias combined with McCune-Albright Syndrome, a one percent malignance-turing chance exists. According to a 1999 study by Dr. Blanco in France, the influence factors may be associated with higher growth hormone secretion.
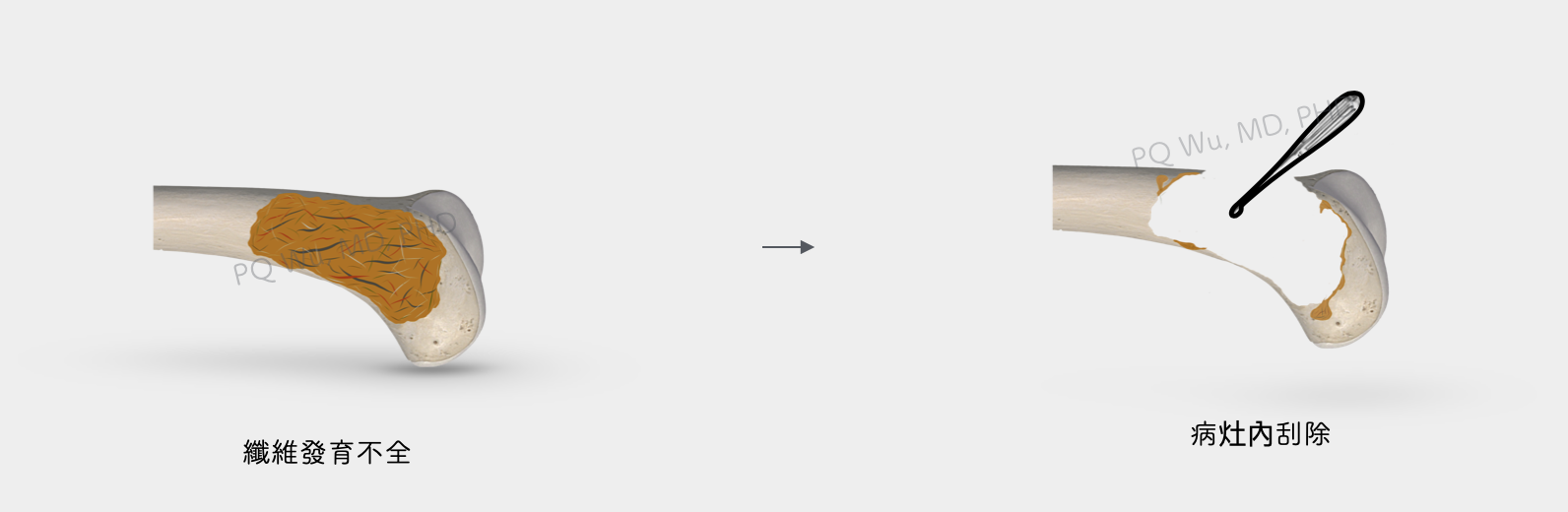
Most fibrous dysplasia won't need surgical treatment. However, if the tumor locates close to the proximal femur near the hip joint, its range is relatively large, and th bone structure becomes more porous, causing pathological fractures easily; we will generally recommend surgical treatment to avoid subsequent complications.
The procedure has two steps: tumor removal and bone transplantation. We'll discuss more in the following articles, respectively. The access links are as follows:
Regular post-surgical outpatient tracking is required. The doctor will determine how much force you can step on and when you can be free from crutches based on how well your bones recover. After full recovery, there's a chance of recurrence of fibrous dysplasia, and regular X-ray checks will still be needed so as to detect and treat problems early.