Bone tumors, often like termites, erode our bones (pillars) into a large hole. After we use a variety of methods to remove these tumors, we have to fill the hole so that the bone structures can remain stable without causing future pathological fractures.
Bone tumor growth can cause serious bone damages.
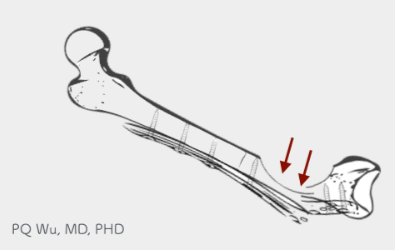
Failure to fill in bone defects can lead to pathological fractures.
The orthopedic surgeon will use different materials to fill the bone cavity after tumor removal. These materials include bone cement (PMMA), artificial bone, allograft bone, and autograft bone.
Bone regeneration, or tissue engineering, is an art of wisdom, and we can only describe it briefly here.
First, we can use a metaphor: If one day Dr. Wu suffered medical disputes and litigations, and he decided to go back to his hometown to cultivate oysters for life. Looking at the empty sea, Dr. Wu must do three things to successfully raise the oysters- constructing the shed, spreading the feed, and allocating the seedlings. Similarly, if we want new bones to grow in bone defects, we must also give the three elements of tissue engineering, which include cells, signals, and scaffolds. Each one is indispensable!
Cells
Cells are like seedlings. The most important cell is the stem cell, and it can differentiate to osteoblast at the bone defects to regenerate new bone tissues. Under normal circumstances, human body will have a significant number of stem cells, and most of us do not need additional supplements to achieve good bone regeneration results.
Signal
Signals are like feeds. The most important ones include bone growth factor (BMP), vascular endothelial growth factor (VEGF), and so on. Under normal circumstances, human body will have a significant number of growth factors, and most of us do not need additional supplements to achieve good bone regeneration results.
Scaffold
Scaffolds are like oyster sheds. Bone defects must need scaffolds like bones to let bone cells grow. For a bone defect after osteosarcoma surgery, we have to add a new ‘shed’ since the original shed has been destroyed. The commonly used tissue scaffolds include bone cement (PMMA), artificial bone, allograft bone, and autograft bone.
Next, let's talk about the differences between these tissue scoffalds.
Bone cement (Poly methyl methacrylate, PMMA) is the best friend of orthopedic doctors! In daily orthopedic surgeries, we will certainly use it. PMMA was invented in 1877 by German scientist Wilhelm Rudolph Fittig. In 1941, it was firstly used by oral surgeons in Alexander Blain Hospital in Detroit for facial reconstruction surgery. Simply put, it's a medical-grade 'acrylate' that is half liquid (which contains unpolymerized MMA) and half powdered (which contains initiators for polymerization) before use.
When used during surgery, the two components are mixed together to trigger the polymerization of MMA to PMMA. In the initial few minutes, PMMA is a glued substance, and after around ten minutes, the polymerized PMMA becomes exothermic, starts swelling, and eventually transforms into a stone-like substance.
The most common use of PMMA is in our artificial knee surgery, where doctors use PMMA to fix artificial joints and bones. In addition, in some orthopedic infections, such as artificial joint infection, myelitis, etc., we can put high concentrations of antibiotics in PMMA and let them gradually release in the body to kill bacteria. In addition, the common use of PMMA is to fill the bone defects.
The greatest advantage of using PMMA is that it provides 'immediate' and 'sufficient' support. Patients with general bone defects filled by PMMA can go and walk right after surgery! The surgery is fast and cheaper. (Of course, there are some other special PMMA on the market, such as with the addition of antibiotics, contrast agents, etc., and they are more expensive and not reimbursed by the National Health Insurance).
Another feature is the advantage and disadvantage, which is 'exothermic'. Based on in vitro test results, PMMA can reach core temperatures between 70 and 120 degrees Celsius during polymerization (**). In human in vivo tests, temperatures can be ranged from 48(**) to 56(***) degrees Celsius. For such a short period of high temperature in the body, bone cells and surrounding tissues will suffer some temporary damage, but the possible residual tumor will also be eliminated.
Still, use PMMA to fill bone defects bring one unfavorable feature, which is its non-bio-degradability. Normally, best bone defect filling material must be metabolized in the human body after a few months or years. In the process of metabolism, bone tissue will gradually regrow.
However, PMMA cannot be metabolized by the body, and such results cannot be achieved. Basically, if we use PMMA to fill the bone defects, such a piece of PMMA will persist, and new bones won’t grow. Because of this limitation, we use it clinically in patients who 'need to bear the weight early'. For younger patients, PMMA is generally not recommended as a bone filler.
* DiPisa JA, Sih GS, Berman AT. The temperature problem at the bone-acrylic cement interface of the total hip replacement. Clin Orthop 1976;121:95-8.
** Harving S, Soballe K, Bunger C. A method for bone-cement interface thermom- etry: an in vitro comparison between low temperature curing cement Palavit, and Surgical Simplex P. Acta Orthop Scand 1991;62:546-8.
*** Linder L. Reaction of bone to the acute chemical trauma of bone cement. J Bone Joint Surg [Am] 1977;59:82-7.
Artificial bones are generally marketed in a wide variety, including calcium sulfate, tricalcium phosphate (TCP), and Hydroxyapatite (HA). These artificial bones are made of materials similar to bone compositions, and they are processed in a 3D stereo porous structure similar to the bone to fill in the bone defects. Depending on the material, the artificial bone will usually be metabolized and replaced with the newly generated bone tissue in the body after about a few months to a year or two.
In our clinical experience, the effectiveness of artificial bone is quite good! However, the cost of artificial bone is quite expensive, and the cheapest one costs about 7000 to 8000 NTD for 10CC. The reimbursement policy of National Health Insurance regulates the different amounts of payments according to the tumor size.
In recent years, more artificial bones with different functions have been launched on the market. Some contain growth factors that can accelerate bone growth, and others can be injected to make bone cavities filled more thoroughly and quickly. Still, the price of these artificial bones is even higher!
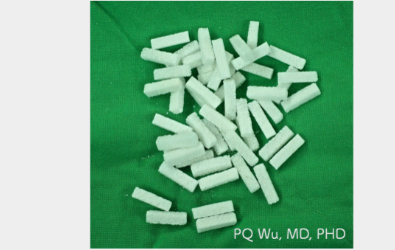
Artificial bones reimbursed by National Health Insurance which contains calcium sulfate and HA
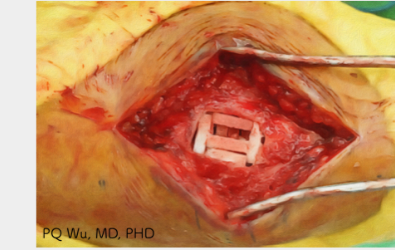
Surgical application of artificial bones to fill bone cavitie
Allograft bones, as the name suggests, refer to 'bones from other people'. Common sources of allograft bones are:
I. Patients with hip disease (fractures, degenerative arthritis, etc.) removed normal femurs during surgery. Since the patient no longer needs this 'normal femur', it is kindly donated.
II. Patients with degenerative arthritis on their knee joint. When they receive joint replacement surgery, part of the normal bone is removed. Since this 'normal bone' is no longer needed by the patient, it is kindly donated
III. The donation of bones from the patients passed away.
For most benign bone tumor bone defects, we use the first and second allograft bones for transplantation. Like artificial bones, these transplanted allograft bones are gradually absorbed by the body, and then new bones will gradually regrow.

The allograft bone donated by a patient with hip fractures

The use of allograft bone to fill the bone cavity during surgery
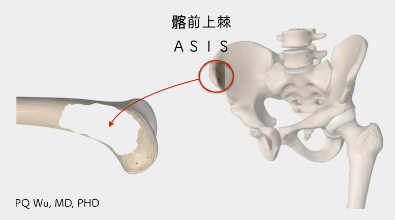
As mentioned before, the best bone transplantation material must have the three elements of tissue engineering- Cells, Signals, and Saffold. The only material that meets these three criteria is ‘autograft’. Autograft bone uses the rarely used bones taken from the patient to fill the bone cavity in the same surgery.When choosing autograft bones, general practitioners will take the patient's bone from the anterior superior iliac spine (ASIS) since this part of the bone is at the axial skeleton and has a less fat content and better effectiveness. The bones just removed have fresh bone cells, stem cells, and various growth factors. If we quickly transplanted them back into the bone defects, very good bone growth results will likely be achieved. Unfortunately, it’s clinical use is limited because taking the bone can cause pain in the patient (even worse than where the tumor is opened), and the amount taken is usually not sufficient to fill the bone defects
Except for PMMA transplantation, other grafts, including artificial bones, allograft bones, or autograft bones, could not bear too much weight in the early stage. The patients have to wait until a few months later, when their new bones are gradually formed and started to align regularly, to bear weight completely. Therefore, regular X-ray examination must be followed every four to six weeks after surgery so that the physicians can understand the situation of bone growth. According to our clinical experience, it generally takes about four to six months for patients to resume running, playing ball, or other more intense sports.