Chondrosarcoma is the second most common primary malignant bone tumor (primary bone sarcoma) after osteosarcoma. The difference with osteosarcoma is that chondrosarcoma occurs mostly in middle-aged people, and the course of the disease is less likely to metastasize distally than other malignant bone tumors. Because chondrosarcoma is not very responsive to chemotherapy, most cases only need surgical removal without the pre- and post-operative chemotherapy. We’ve made a comparison of these two common malignant bone tumors:
Chondrosarcoma
- Most cases are above 50 years old
- The second most common primary malignant bone tumor
- Most are a low-level malignancy
- Chemotherapy is not effective
- Radiation therapy is not effective
Osteosarcoma
- More cases are between 10 to 20 years old
- The most common primary malignant bone tumor
- Mostly highly malignant
- Chemotherapy is effective
- The effectiveness of radiation therapy is general
Chondrosarcoma can be divided into many different types, and 90% of which are conventional chondrosarcoma. In this article, we describe 'conventional chondrosarcoma' mostly. Other rare types of chondrosarcoma differ significantly in clinical performances and prognosis with conventional chondrosarcoma, and we’ll describe them at the end of the article.
Although chondrosarcoma is a malignant tumor, most patients may have no symptoms initially since it grows slow. After a few months or years, patients may begin to feel 'hidden pain' or 'touch the lump' and have other symptoms. Especially at the pelvic, since it’s deep, most patients cannot touch the lump. Also, the patients’ symptoms and ages are like spinal disc problems; hence, it’s not easy to diagnose clinically. Often the tumor has grown quite large when the patient finds out!
Chondrosarcoma is a more common malignant bone tumor. Among primary malignant bone tumors, the chance of occurrence is second, only behind malignant osteosarcoma. According to the statistics from Mayo Center in the United States, it takes about 20% of primary malignant bone tumors, which is about 0.7 times the number of malignant osteosarcomas. However, in our observation, malignant chondrosarcoma occurred at a lower rate in Asian populations; generally, the proportion found clinically is lower than in Europe and the Americas.
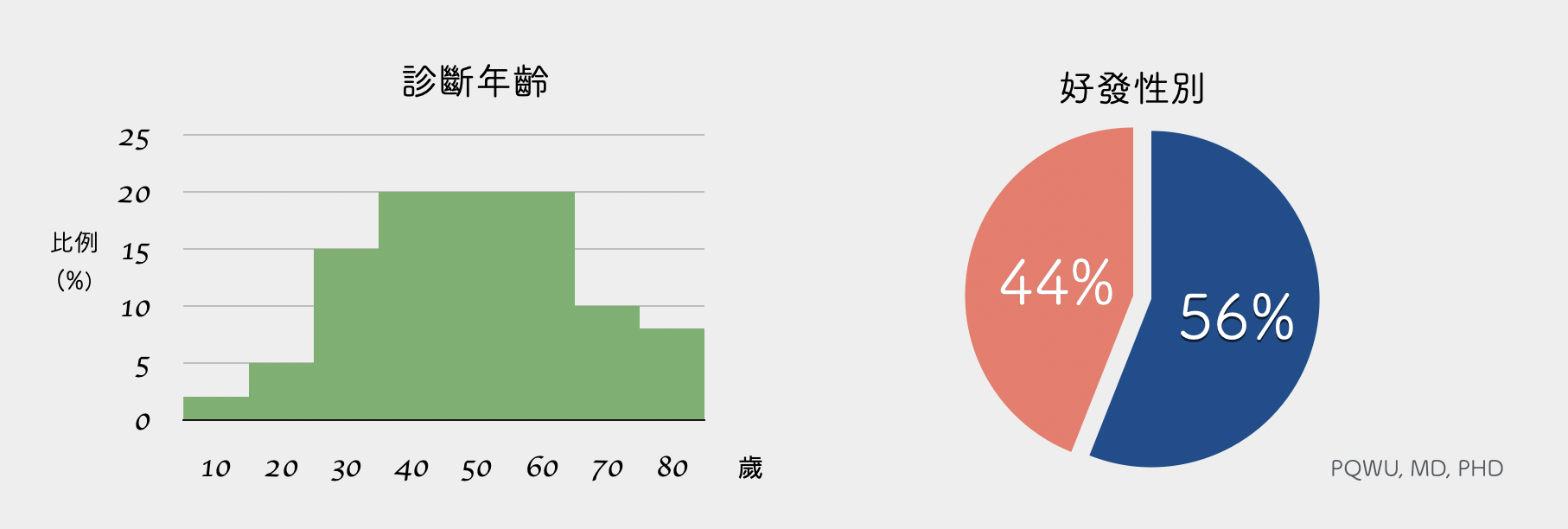
Chondrosarcoma is different from the general primary malignant bone tumor. It is likely to occur in adolescents but more likely to occur in middle-aged people. On average, about 40 to 60 years old is the peak age range for chondrosarcoma occurrence. The sex ratio is higher for men, taking about 56%.
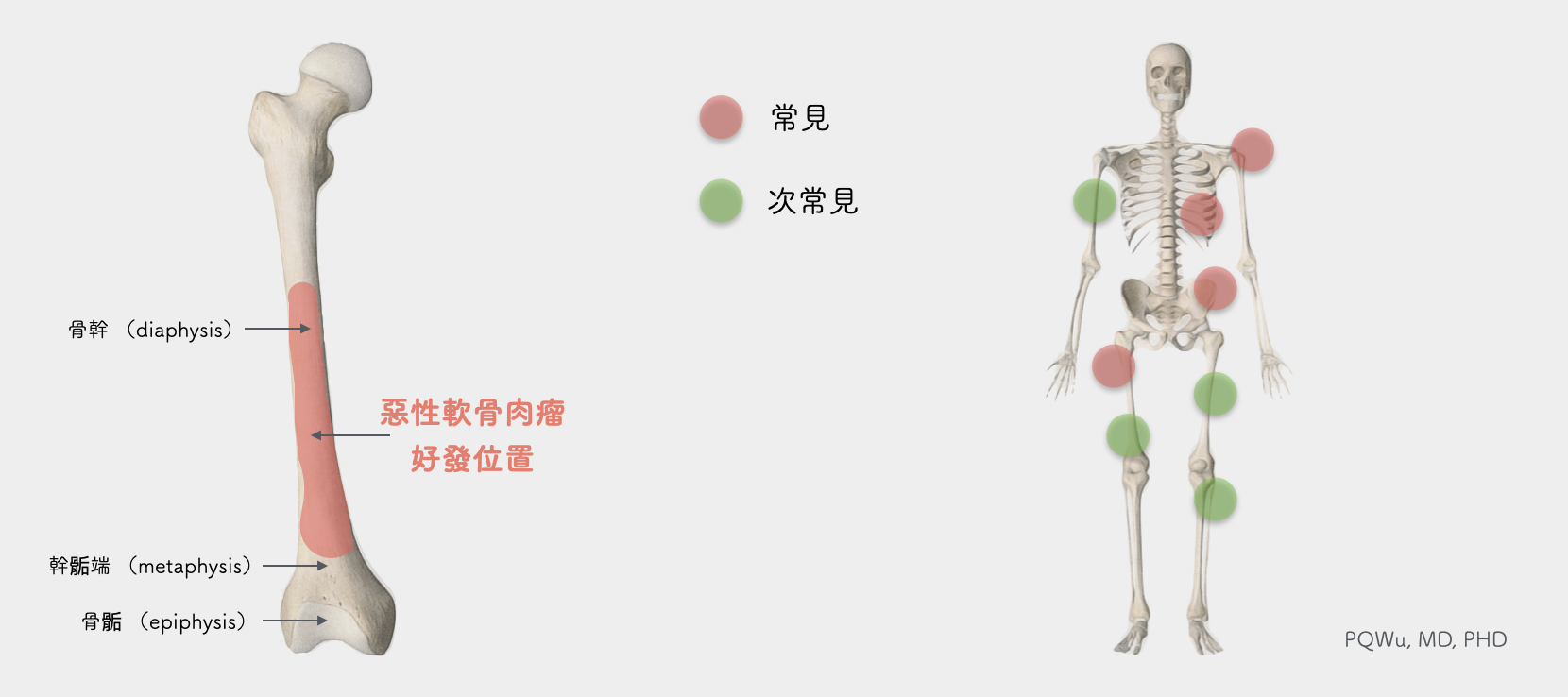
Chondrosarcoma is more likely to occur near the axial bone, such as the pelvis, ribs, and shoulder blades. In addition, the locations close to limbs such as the proximal tibia (shoulder) and proximal femur (hip) are also quite common positions. Also, because most of these locations are the passages of important nerves and blood vessels and the origin of many muscles, it is easier to affect the patient's limb function after surgical removal.
Most of the malignant chondrosarcoma that primarily grows at metaphysis will extend to the diaphysis. Hence, clinically, we often see malignant chondrosarcoma that extends along the bone marrow cavity for a considerable amount of range. More specially, we occasionally will also see chondrosarcoma grow on the fingers or toes clinically.
Most X-ray images of chondrosarcoma have considerable specificity. For example, there is an endosteal scalloping phenomenon, a little calcification, and the growth along the bone marrow cavity to the backbone. But these phenomena are mostly like benign endogenous cartilage. Especially for low-level malignant chondrosarcoma, it is often not distinguished by X-rays or even MRI. It is not easy to distinguish malignant chondrosarcoma until it progresses to cortical destruction or soft tissue extension. Therefore, it is quite difficult for clinicians to determine the initial chondrosarcoma.
The cause of primary chondrosarcoma is unknown. However, if it’s secondary chondrosarcoma, the cause is most likely from the transformation of benign bone tumors such as osteochondroma, enchondroma, etc.
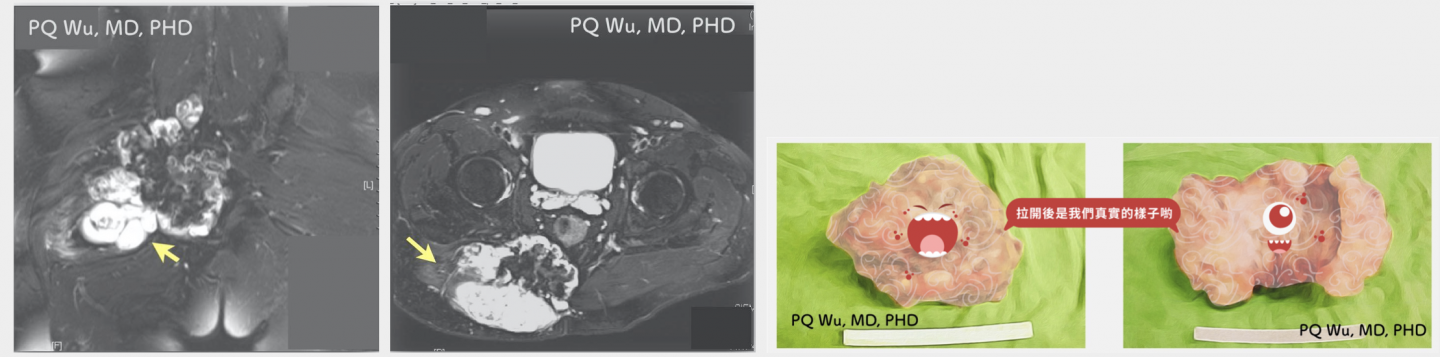 The chondrosarcoma at the pelvis turned into a malignant chondroma ten years later.
The chondrosarcoma at the pelvis turned into a malignant chondroma ten years later.
Chondrosarcoma has quite a variety of classifications. According to the World Health Organization (WHO) classification, it can be divided into several categories:
Chondrosarcoma: WHO classification
Conventional Chondrosarcoma
About 90% of chondrosarcoma is conventional chondrosarcoma. It can be divided into primary chondrosarcoma and secondary chondrosarcoma. Our previous descriptions illustrate mainly this type of chondrosarcoma. The secondary chondrosarcoma refers to chondrosarcoma that is transformed by other benign bone tumors such as common osteochondroma.
Mesenchymal chondrosarcoma
Mesenchymal chondrosarcoma is quite rare. The biggest feature is that it occurs at a lower age than conventional chondrosarcoma. Most of the cases occur in young people at the ages of 20 to 30 years old. The overall prognosis is poor, with an average five-year survival rate of about 54% and an average 10-year survival rate of about 28%.
Dedifferentiated chondrosarcoma
About 10% of chondrosarcoma is dedifferentiated chondrosarcoma. ‘Dedifferentiated’ typically refers to the chondrosarcoma tissue mixed with other undifferentiated tumor cells such as part of original osteosarcoma cells, original fibrosarcoma cells, etc. So, some doctors think it should be called 'chondrosarcoma with additional mesenchymal component.' The prognosis of dedifferentiated chondrosarcoma is quite poor, with an average five-year survival rate of only 10%, making it a rather difficult malignant tumor to treat.
Clear cell chondrosarcoma
It is quite rare, taking about only two percent of chondrosarcoma. Clear cell chondrosarcoma is quite difficult to diagnose correctly since the likely occurrence location is special, mostly in the epiphysis, and its tissue biopsy characteristics are similar to those of the two benign bone tumors in chondroblasts and osteoblasts. Hence, it is mostly misdiagnosed initially as benign bone tumors, resulting in a poor overall prognosis.
Periosteal chondrosarcoma
It is quite rare, taking about two percent of chondrosarcoma. It is very easy to be misrecognized as benign bone tumors.
Extraskeletal myxoid chondrosarcoma
Compared to other types of chondrosarcomas, Extraskeletal myxoid chondrosarcoma is not grown from the bones but the surrounding muscles or connective tissue. Thus, it can be classified as soft tissue sarcoma.
Grade I, Low-grade
Most conventional chondrosarcoma is either grade I or II. The grade I chondrosarcoma is not easily distinguished from benign enchondroma in both histology and imaging. Therefore, clinicians often have to determine based on experiences such as the patient's medical history, symptoms, tumor location, and tumor growth rate.
Grade II, Intermediate-grade
Most conventional chondrosarcoma is either grade I or II. Grade II chondrosarcoma begins to have increased cellularity, increased nuclear size, and distinct nucleoli. Most myxoid chondrosarcoma is classified as phase II chondrosarcoma.
Grade III, High-grade
It is rare and has a poor prognosis. Grade III chondrosarcoma grows rapidly and is likely to have distal metastasis. Mesenchymal chondrosarcoma and dedifferentiated chondrosarcoma are both phase III chondrosarcoma.
Most chondrosarcomas (conventional or phase I and II) rarely metastasize distally. However, the phase III (highly malignant) chondrosarcomas have half the chances to metastasize distally and result in a poor prognosis.
Generally, chemotherapy and radiation therapy are ineffective for chondrosarcoma; hence, ‘surgery’ is the most important treatment for chondrosarcoma, and chemotherapy is unnecessary. However, we will still recommend chemotherapy for highly malignant chondrosarcoma if the patient is young, though not effective as for osteosarcoma, to enhance the prognosis.
The choice of surgery for chondrosarcoma has a considerable relationship with its pathological phases, which we describe below:
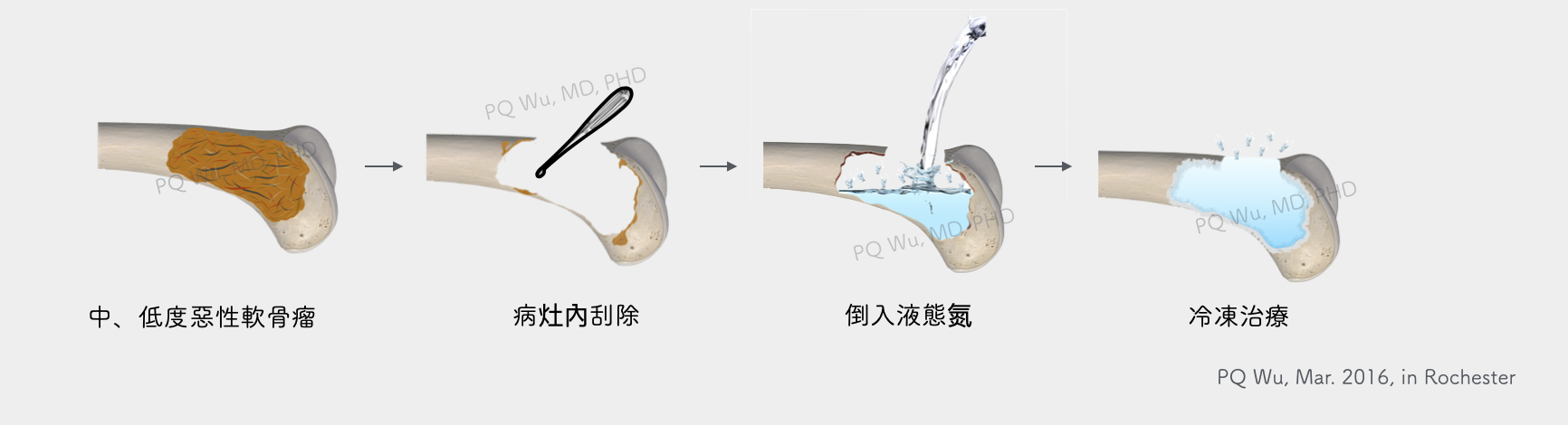
Suppose it is for the phase I (low malignancy) or phase II at a specific location (moderate malignancy). In that case, we can use intralesional curettage and adjuvant therapy to achieve better limb function retention since the tumors are unlikely to metastasize distally and recur. Here, adjuvant therapy is very important and must be strongly effective methods such as liquid nitrogen or FNEC. If we conduct intralesional curettage without adjuvant therapy, the chance of recurrence will be quite high! For detailed descriptions, please read the articles with the links below.
If the chondrosarcoma is highly malignant, the use of intralesional curettage will have high tumor recurrence. Hence, more complex surgery is recommended- the wide resection. Tumor-type artificial joints or biological bones can reconstruct the bone defects after surgical removal. For detailed descriptions, please refer to the articles below.

Step 1: Highly malignant chondrosarcoma above the knee.

Step 2: Surgery to remove the tumor completely and widely.
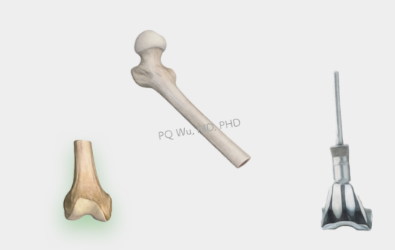
Step 3: Bone reconstruction with biological reconstruction or tumor-type artificial joints.

Step 4: Biological reconstruction to transplant the real bones back into the body.
The overall prognosis of chondrosarcoma is better, and most patients do not need chemotherapy. It is a relatively easy malignant bone tumor to treat. However, if it occurs in the pelvis, it often causes serious loss of limb function and recurs years after surgery since the tumors are often quite large and pelvic surgery is difficult and risky. So, it is important to pay considerable attention overall!