Before we start, I want to clarify that I recognize "Manipulation" as a broad and profound traditional medicine in the Chinese nation. It provides significant help for many disease treatments! However, Same as Western medicine, those drugs which are good and expensive, if used at the wrong time or wrong place, will cause significant side effects!
One day in 2006, when I was a second-year resident, my teacher, Professor WM Chen, suddenly asked me: "Po-Qui, have you ever observed that some patients with osteosarcoma seem to have received manipulation, and it seems that their treatment results are not good. I suggest that you investigate it." Therefore, on the one hand, when we encountered new osteosarcoma patients, we reminded them seriously; on the other hand, we began large-scale, statistical investigation. Eventually, after a year, we reached our preliminary conclusion. In the fall of 2007, we reported our study results at the Taiwan Orthopaedic Association and the International Society of Limb Salvage, ISOLS. In 2010, the comprehensive findings were published in the prestigious journal- Journal of Bone and Joint Surgery, British. (Note I)
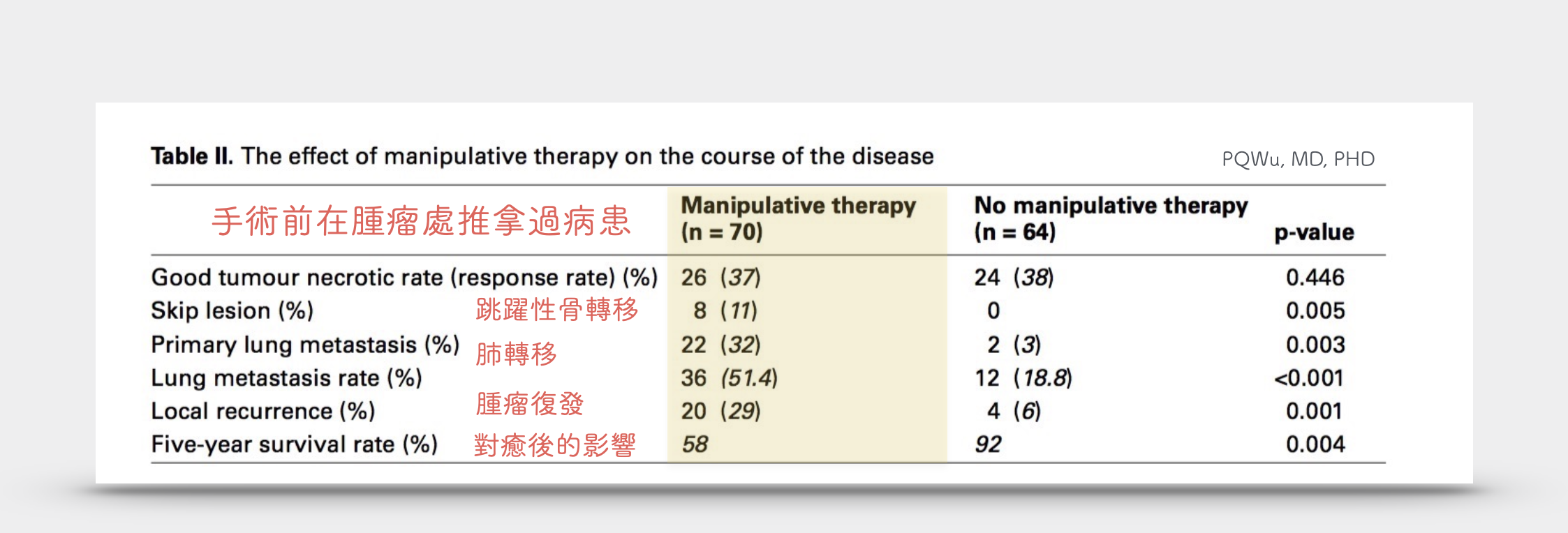
According to our research, in Taiwan, before their Osteosarcomas were diagnosed, 52% of patients seeked Chinese manipulation in Chinese physiotherapists or doctor's offices. They mistakenly thought their pains are from muscle aches or growing pains. These patients had poor prognoses, higher lung metastasis rates, and higher local recurrence rates after surgery than patients with osteosarcoma who had not received a manipulation.
2010年,刊登在著名骨科雜誌 Journal of Bone and Joint Surgery, British
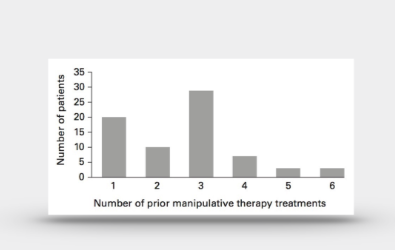
平均手術前推拿的次數
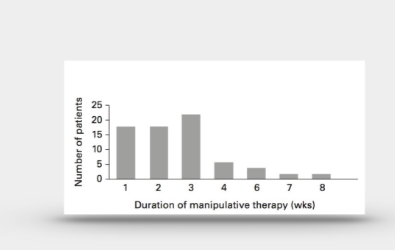
平均手術前推拿的週數
We evaluated the long-term outcome of patients with an osteosarcoma who had undergone prior manipulative therapy, a popular treatment in Asia, and investigated its effects on several prognostic factors. Of the 134 patients in this study, 70 (52%) patients had manipulative therapy and 64 (48%) did not. The age, location, and size of tumour were not significantly different between the groups. The five-year overall survival rate was 58% and 92% in the groups with and without manipulative therapy (p = 0.004). Both the primary and overall rates of lung metastasis were significantly higher in the manipulative group (primary: 32% vs 3%, p = 0.003; overall lung metastasis rate: 51.4% vs 18.8%, p < 0.001). Patients who had manipulative therapy had higher local recurrence rates in comparison to patients who did not (29% vs 6%, p = 0.011). The prognosis for patients with osteosarcoma who had manipulative therapy was significantly poorer than those who had not. Manipulative therapy was an independent factor for survival. This form of therapy may serve as a mechanism to accelerate the spread of tumour cells, and therefore must be avoided in order to improve the outcome for patients with an osteosarcoma.
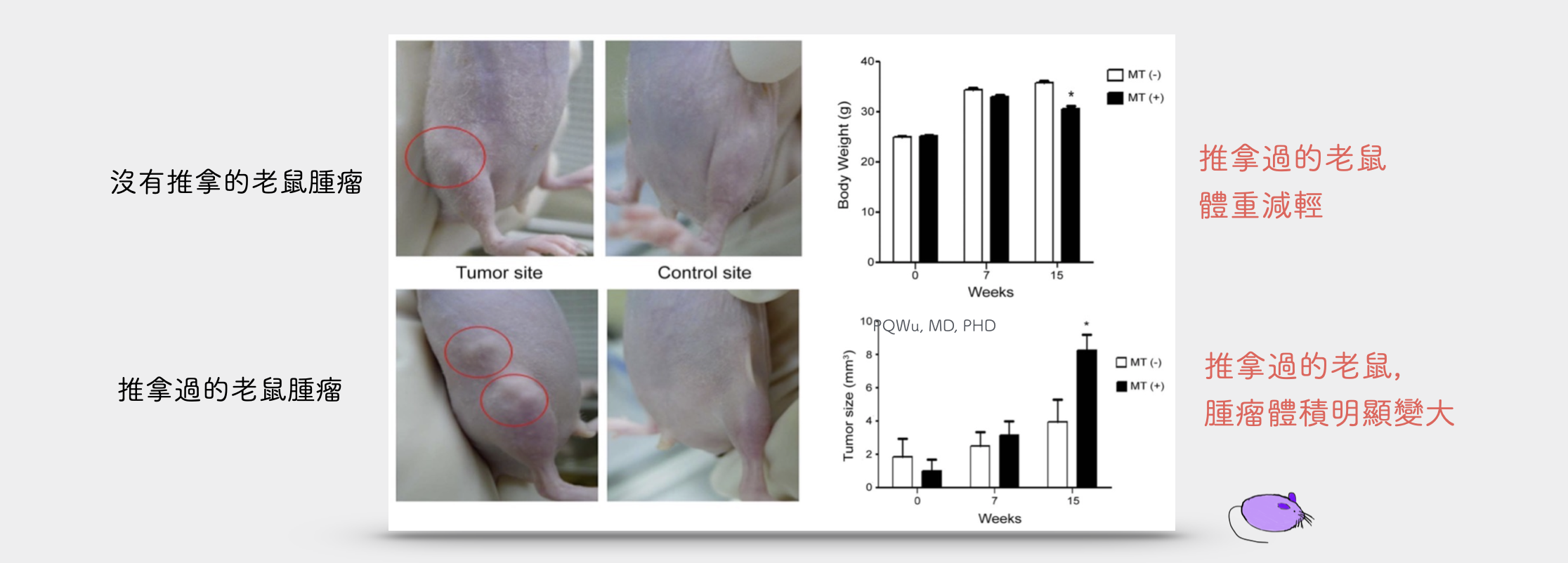
In addition, we have also conducted fundamental experiments and animal experiments to avoid bias from clinical retrospective studies. We implanted the MG-63 osteosarcoma cell line into the mice and manipulated them. After fourteen days, MG-63 Osteosarcoma cells were found in the lungs of the mice. The MMP-9 biomarker, which represents the incurred metastasis, was much higher than that of the mice that had not been manipulated. We published the conclusion in ISOLS in 2011 and PLoS One in 2014. (Note 2)
2014年,刊登在著名骨科雜誌 PLOS one
Both our clinical observations and laboratory animal studies have shown that pre-surgical manipulation at lesions can have a considerable impact. Therefore, we would like to recommend that if you know people suspected or confirmed suffering from osteosarcoma or other bone tumors, please remind them not to seek manipulation, hot compress, and acupuncture cupping, or other acts to prevent the spreading of the tumor mechanically.
Note 1:
The prognosis for patients with osteosarcoma who have received prior manipulative therapy. Bone Joint J. 2010;92-B(11):1580-1585.
Note 2:
Manipulation therapy prior to diagnosis induced primary osteosarcoma metastasis--from clinical to basic research. Tang C-H, ed. PLoS ONE. 2014;9(5).