Lung cancer is a fairly common cancer. It ranks the third among all cancers, after breast and colorectal cancer, according to the top 10 cancer data in Taiwan released by the Taiwan CDD in 2015.
by PQ WuBones are the organs most susceptible to distal metastasis in lung cancer patients. Literature reports showed that 20% of patients had combined bone metastasis at the time of being diagnosed as lung cancer (*). According to a 1982 autopsy study (**), when the disease was servere, 40% of the cases would occur bone metastasis, 30% would have chest cavity metastasis, 20% would have lymphatic metastasis, and 15% of them would have liver and brain metastasis.
As with most bone metastasis, bone metastasis of lung cancer occurs most often in the spine (53%), ribs (45%) and limbs (16%). Because the overall lung cancer progress is faster, and the initial bone metastasis has no obvious unique symptoms, many patients will already have multiple bone metastasis when the metastasis is found! Even in our clinical observations, many lung cancer bone metastasis are found only after the emergency room visit for pathogenic fractures!
**Lung Cancer: Clinical Diagnosis and Treatment, 2nd edn. Grune and Stratton: New York, 1982: 185-200
Risk factors for concurrent lung cancer bone metastasis
What conditions are lung cancer patients more likely to have bone metastasis? The main factors are the type of lung cancer. For the more severe lung cancer, different metastasis ratios exist (*):
1. Small cell carcinoma has about a 70% chance of bone metastasis, which is the highest of all lung cancer types.
2. Prostate cancer has about a 45% chance of bone metastasis, which is the second highest of all lung cancer types.
3. Large cell carcinoma has about a 25% chance of bone metastasis.
4. Squamous cell carcinoma has about a 15% chance of bone metastasis, which is the lowest of all lung cancer types.
* Lung Cancer: Clinical Diagnosis and Treatment, 2nd edn. Grune and Stratton: New York, 1982: 185-200.
Hypercalcemia of malignancy is a paraneoplastic syndrome of cancer patients. Most occur in patients with lung, breast and multiple myeloma. The main light symptoms are loss of appetite, nausea, constipation, abdominal pain, thirst, frequent urination, weakness, muscle aches, and headaches. In severe cases, it would cause kidney stones, irregular heart rhythms, fainting, and coma. The main causes of malignant hypercalcemia are PTHrP (parathyroid hormone-related protein) secreted by tumor cells or a small amount of 1,25-dihydroxyvitamin D and parathyroid. These hormones act on the bones and kidneys separately to increase the release of calcium ions from the bones and reduce their excretion.
The chance of hypercalcemia of malignancy is quite different in literature at present. According to a 1993 research at MD Anderson Cancer Center, among a total of 7,667 cancer patients, moderate to severe cases (calcium ion concentration greater than 2.7mmol/l) took only 1.2%. Among them, kidney cancer was the most, myeloma was the second, undiagnosed cancer was the third, and lung cancer was merely the fourth. However, when the patients had advanced cancers, the chance of malignant hypercalcemia increased to 20-40% (*). In another study, it was found that lung and breast cancer accounted for more than half of all cases (**). There are also studies suggesting that lung cancer has a 35% chance of developing malignant hypercalcemia (***).
In mild malignant hypercalcemia, we can advise patients to hydrate and exercise more. In severe cases, medications such as bisphosphonates, XGEVA, and steroids are needed.
* Incidence of hypercalcaemia in patients with malignancy referred Lo a comprehensive cancer center. Cancer 1993; 71: 1309-12.
**Hypercalcaemia-a hospital survey. Qu J Med 1980; 196: 405-18.
***Overview of cancer-related hypercalcaemia: epidemiology and etiology. Semin Oncol 1990; 17(sllppl 5): 3-9.
Once lung cancer patients are unfortunately suffering from bone metastasis, they have a high chance of combing 'skeletal-related events, SRE', which can have a significant impact on them (*, **). SRE refers to the occurrence to patients by bone metastasis, which accounts for about 20% each.
1. Spinal cord compression. Bone metastasis of lung cancer and breast cancer is the most likely one to cause nerve compression in the spine.
2. Pathological fractures.
3. Reception of radiation to bone or bone surgery because of the presence of clinical symptoms, e.g., pain.
The tumor cells metastasized to the bone can produce pain by the induction of hormones such as bradykinin, interleukin-6 (IL-6), granulocyte-macrophage colony-stimulating factor, and tumor necrosis factor. The cells will also promote the growth of osteoclast and drive local bone destruction, resulting in subsequent severe pathological fractures. For detailed descriptions of this section, readers can click through the links below.
* Natural history of skeletal-related events in patients with breast, lung, or prostate cancer and metastases to bone: a 15-year study in two large US health systems. Support Care Cancer 2013; 21: 3279–86.
** Natural history of skeletal-related events in patients with breast, lung, or prostate cancer and metastases to bone: a 15-year study in two large US health systems. Support Care Cancer 2013; 21: 3279–86.
Clinically, if bone metastasis is discovered in lung cancer, the subsequent radiation, surgery, or both will be determined based on the location of the tumor, the internal medical situation, and the prognosis to improve limb pains and avoid pathological fractures. However, since we know that cancer patients have weaker physical strength and overall body condition than the general public, the indications requiring surgery are different. So, when will surgery be required? Please read the article below for a detailed description.
The surgery for lung cancer combined with bone metastasis can be divided into two methods according to the purpose:
Thorough cure (wide resection of tumor)
If it is a solitary bone metastasis or is for a patient with a good prognosis, we will treat it as a primary bone tumor and conduct wide resection, and hope to cure it thoroughly.
Reduce pain (intralesional curettage)
Suppose the bone metastasis is transferred to multiple parts of the body or is expected to have a worse prognosis. In that case, we will perform intralesional curettage to ensure faster recovery and lower surgical risk.
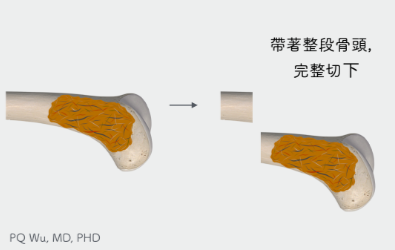
Wide Resection .
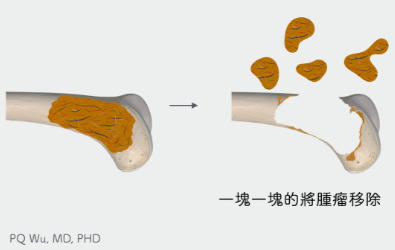
Intralesional Curettage
First. For patients with solitary bone metastasis or a good prognosis, wide resection and limb reconstruction will be conducted as we treat the metastasis as a primary bone tumor and hope to cure it.
Second. In the case of bone metastasis to multiple parts of the body or patients who are expected to have a poor prognosis, intralesional curettage is used. In addition, depending on the surgical situation, adjuvant therapy will be considered to reduce tumor recurrence.
The bone cavity leftover from the tumor removal will be reconstructed with autograft, allograft, artificial bones, or artificial joints, hoping to alleviate patients’ pain and avoiding complications of pathological fractures.
(Figure 1) However, because intralesional curettage will have a fairly high tumor recurrence rate (local recurrence), post-surgical radiation therapy will generally be conducted. However, radiation therapy has certain risks, including wound infection, low blood production, and the influence on peripheral organs.
For a detailed description of the surgery, please read our article below:
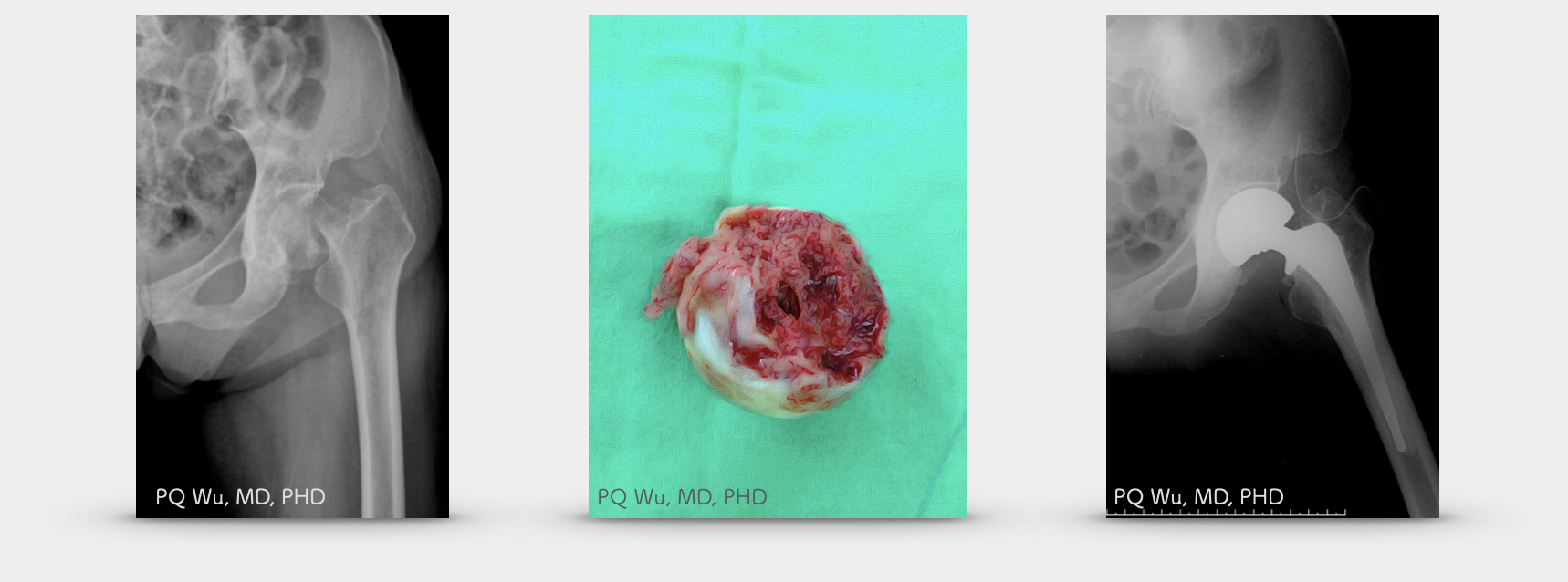
The X-ray image below is the image of a 70-year-old woman with lung cancer and suffering bone metastasis at the left neck of the femur combined with pathological fracture. After removing the tumor and treating it with a semi-artificial hip joint, the patient can get out of bed the next day after the surgery.
Lung cancer combined with bone metastasis is a fairly common clinical problem, and the prognosis is quite poor! Both physicians, family members, and patients should be on high alert. For patients with high risk and bone symptoms, appropriate imaging examination should be given, and the risk of pathological fractures should be assessed. If it conforms to the indication of surgical treatment, intervention should be executed as early as possible to avoid subsequent complications. Medication or radiation therapy should be given to improve the quality of life if surgery is not required or feasible. In addition, special care should be taken on the home environment and patient activities to avoid falling that causing follow-up problems!