Prostate cancer is a male-exlusive cancer. The occurrence age is mostly between 60 and 75 years old. According to the top 10 cancer data in Taiwan released by the Taiwan CDD in 2015, it ranks the sixth among all cancers and the fifth among all male cancers.
by PQ Wu
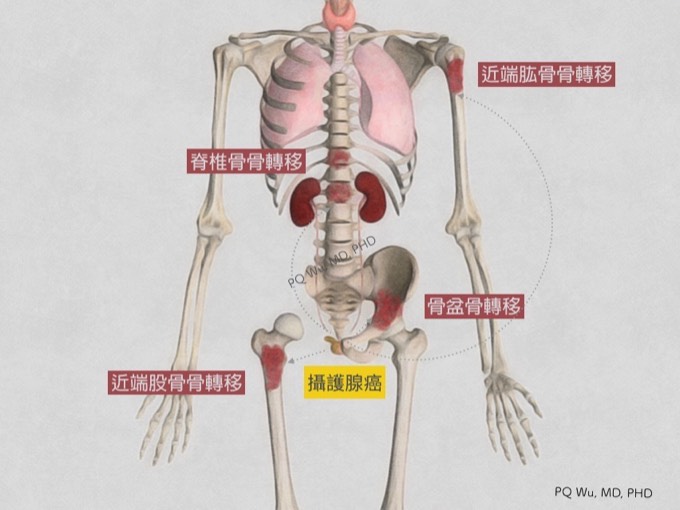
According to a study in 1999 (*), 10% of patients would have bone metastasis when prostate cancer is diagnosed initially, resulting in a fairly poor prognosis. Subsequent bone metastasis are highly related to the stage of cancer. Many research reviews (**~****) reported the possible chances of incurring bone metastasis are as follows:
1. T1/T2 phases: About 3 to 41% would incur bone metastasis.
2. T3/T4 Phases: Approximately 12 to 55% would incur bone metastasis.
If divided by pathological tumor differentiation:
1. Well differentiated: Approximately 3 to 10% would incur bone metastasis.
2. Moderately differentiated: About 13 to 57% would incur bone metastasis.
3. Poorly differentiated: About 42 to 80% would incur bone metastasis.
Since the occurrence rate of prostate cancer is high, and the chance of incurring bone metastasis is relatively high. Hence, prostate cancer combined with bone metastasis is a fairly common problem clinically.
* Cancer statistics. CA Cancer J Clin 1999;49: 8-29.
** Results of conservative management of clinically localized prostate cancer. N Engl J Med 1994; 330: 242-8.
***Fifteen-year survival in prostate cancer: a prospective, population- based study in Sweden. J Am Med Assoe 1997; 277: 467-71.
****Competing risk analysis of men aged 55-74 years at diagnosis managed conservatively for clinically localized prostate canceL J Am Med Assoe 1998; 280: 975-80.
Under what conditions would a prostate cancer patient incur bone metastasis? We can learn from the following studies:
(i) Cancer, 2000. After wide resection of prostate cancer, the risk factors for bone metastasis include (*):
1. Gleason score is equal to or greater than 7 points.
2. Combined invasion to seminal vesicle and lymphatic tissues.
3. Biochemical failure occurs within two years of surgery.
(ii) Urology and Urol Clin N Am, 1997. Two studies found that after radiation therapy for prostate cancer, the risk factors for bone metastasis include (**,***):
1. Gleason score is equal to or greater than 8 points.
2. Pretreating PSA is greater than 20 ng/dl.
3. T3/T4 interphase
4. Combined invasion to lymphatic tissues
5. After radiation therapy, the PSA is still greater than 4 ng/dl
Therefore, for prostate cancer patients who meet the above conditions, both physicians and patients should be more cautious to the possibility of bone metastasis.
* The natural history, skeletal complications, and management of bone metastases in patients with prostate carcinoma. Cancer 2000; 88: 2989-94.
** Serum testosterone: a significant determinant of metastatic relapse for irradiated localized prostate canceL Urology 1997; 49: 327-34.
***Prostate specific antigen after radiation therapy. Urol Clin N Am 1997; 24: 40714.
Most cancers, when combined with bone metastasis, cause osteolysis that generates osteolytic lesion in the X-ray image. For detailed mechanism, you can read through link below.
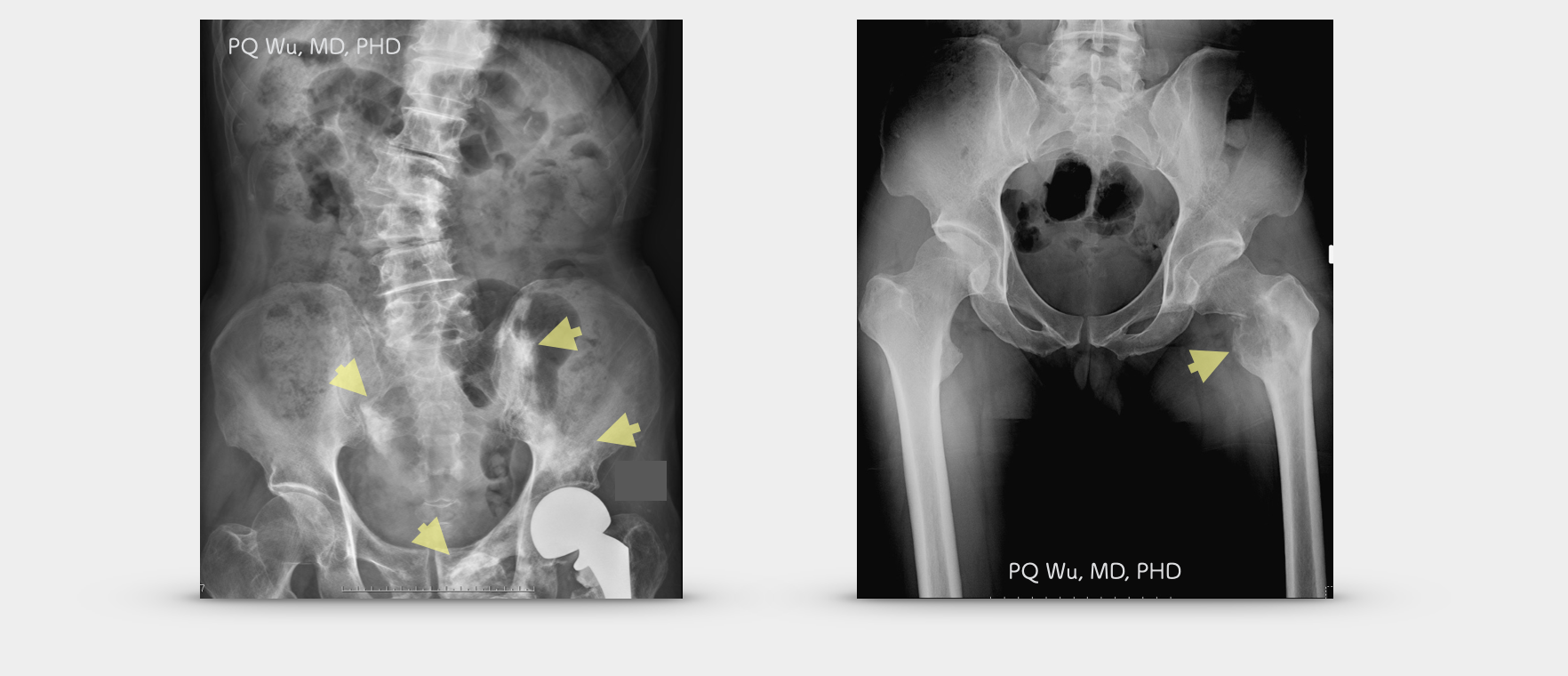
(Top left) General cancer bone metastasis produce osteolytic lesions. (Top right) Bone metastasis for prostate cancer generates osteoblastic lesions.
When bone metastasis ocurred in prostate cancer patients, there is a certain chance to incur skeletal-related events, SRE. Such events will bring considerable impact to these cancer patients (*,**). SRE refers to the occurrence to patients by bone metastasis.
1. Spinal cord compression. Bone metastasis of lung cancer and breast cancer is the most likely one to cause nerve compression in the spine, yet, it is less common in prostate cancer.
2. Pathological fractures.
3. Reception of radiation to bone or bone surgery because of the presence of clinical symptoms, e.g., pain.
The tumor cells metastasized to the bone can produce pain by the induction of hormones such as bradykinin, interleukin-6 (IL-6), granulocyte-macrophage colony-stimulating factor, and tumor necrosis factor. The cells will also promote the growth of osteoclast and drive local bone destruction, resulting in subsequent severe pathological fractures. For detailed descriptions of this section, readers can click through the links below.
Clinically, if bone metastasis is discovered in prostate cancer, the subsequent radiation, surgery, or both will be determined based on the location of the tumor, the internal medical situation, and the prognosis to improve limb pains and avoid pathological fractures. However, since we know that cancer patients have weaker physical strength and overall body condition than the general public, the indications requiring surgery are different. So, when will surgery be required? Please read the article below for a detailed description.
The surgery for prostate cancer combined with bone metastasis can be divided into two methods according to the purpose:
Thorough cure (wide resection of tumor)
If it is a solitary bone metastasis or is for a patient with a good prognosis, we will treat it as a primary bone tumor and conduct wide resection, and hope to cure it thoroughly.
Reduce pain (intralesional curettage)
Suppose the bone metastasis is transferred to multiple parts of the body or is expected to have a worse prognosis. In that case, we will perform intralesional curettage to ensure faster recovery and lower surgical risk.
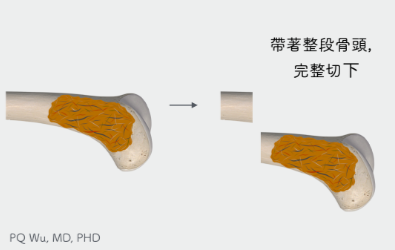
Wide Resection
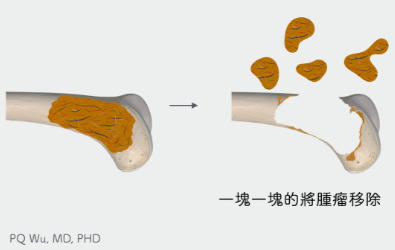
Intralesional Curettage
First. For patients with solitary bone metastasis or a good prognosis, wide resection and limb reconstruction will be conducted as we treat the metastasis as a primary bone tumor and hope to cure it.
Second. In the case of bone metastasis to multiple parts of the body or patients who are expected to have a poor prognosis, intralesional curettage is used. In addition, depending on the surgical situation, adjuvant therapy will be considered to reduce tumor recurrence.
The bone cavity leftover from the tumor removal will be reconstructed with autograft, allograft, artificial bones, or artificial joints, hoping to alleviate patients’ pain and avoiding complications of pathological fractures.
(Figure 1) However, because intralesional curettage will have a fairly high tumor recurrence rate (local recurrence), post-surgical radiation therapy will generally be conducted. However, radiation therapy has certain risks, including wound infection, low blood production, and the influence on peripheral organs.
For a detailed description of the surgery, please read our article below:
Prostate cancer combined with bone metastasis is a fairly common clinical problem. Both physicians, family members, and patients should be on high alert. For patients with high risk and bone symptoms, appropriate imaging examination should be given, and the risk of pathological fractures should be assessed. If it conforms to the indication of surgical treatment, intervention should be executed as early as possible to avoid subsequent complications. Medication or radiation therapy should be given to improve the quality of life if surgery is not required or feasible. In addition, special care should be taken on the home environment and patient activities to avoid falling that causing follow-up problems!