Fibroid tumor is a fairly rare tumor. Although it’s essentially a benign soft tissue tumor, it doesn’t have a clear boundary between normal tissues. Hence, it very likely to recur after surgery. For physicians specialized in osteosarcoma, it is a difficult and complex disease
Other names
Chinese: 纖維類瘤,硬纖維瘤,類結締織瘤
English: Desmoid tumor, Aggressive fibromatosis. “Desmos” means “Tendon-like” in Greece.
Symptoms
Fibroid tumor has a symptom of hard lumps that patients can easily touch at the tumor site. Since tumors grow slowly and usually located in deeper muscles, they are generally not easy to be detected. If the tumor continues to grow large, it can limit the patient's activity. On average, the tumor size is about 7 centimeters at the time of diagnosis.
The growth of fibroid tumors has two completely different characteristics. The first is 'self-limitation’, which means that the tumor will stop growing when the tumor grows or recurs for a while. It does not disappear but reaches a stable state. The patient will not have any particularly uncomfortable symptoms at this time.
In another case, the tumor continues to grow, constantly damaging normal muscle tissue. This condition can cause serious functional impairment and can be troublesome.
About 50% of patients' tumor growth would gradually stop after a period of tracking time, and 20% of patients would have tumors shrunk slightly, according to a backward study (*) published in the Journal of Clinical Oncology in 2011 by a pathologist at Institut Bergonié in France. The remaining 30% would continue to grow.
In another study at Kyoto University (**), researchers collected data on 11 patients. Two of whom underwent surgeries during the tracking process. Among eight of the other nine patients, seven of whom had stable tumor size without increase after tracking for an average of 56 months. However, one of them had a tumor volume increased rapidly to more than 30 centimeters!
Unfortunately, in current medical care, we are not able to use specific methods to 'guess' the future development of tumors! As a result, clinicians are not likely to decide on the 'most appropriate’ treatment for patients.

*Prognostic Factors Influencing Progression-Free Survival Determined From a Series of Sporadic Desmoid Tumors: A Wait-and-See Policy According to Tumor Presentation. J Clin Oncol. 2011;29(26):3553-3558.
**Nakayama T, Tsuboyama T, Toguchida J, Hosaka T, Nakamura T. Original article Natural course of desmoid-type fibromatosis. Journal of Orthopaedic Science. 2008;13(1):51-55. doi:10.1007/s00776-007-1187-1.
Incidenc
The incidence of fibroid tumors is low. Two to four cases occur in about 1 million population. Across Taiwan, we estimate about 60 to 100 patients. At the therapeutical and Research Center of Musculoskeletal Tumor in Taipei Veterans General Hospital, an outpatient clinic would discover a new patient in about six to 12 months. It is relatively rare in all benign soft tissue tumors.
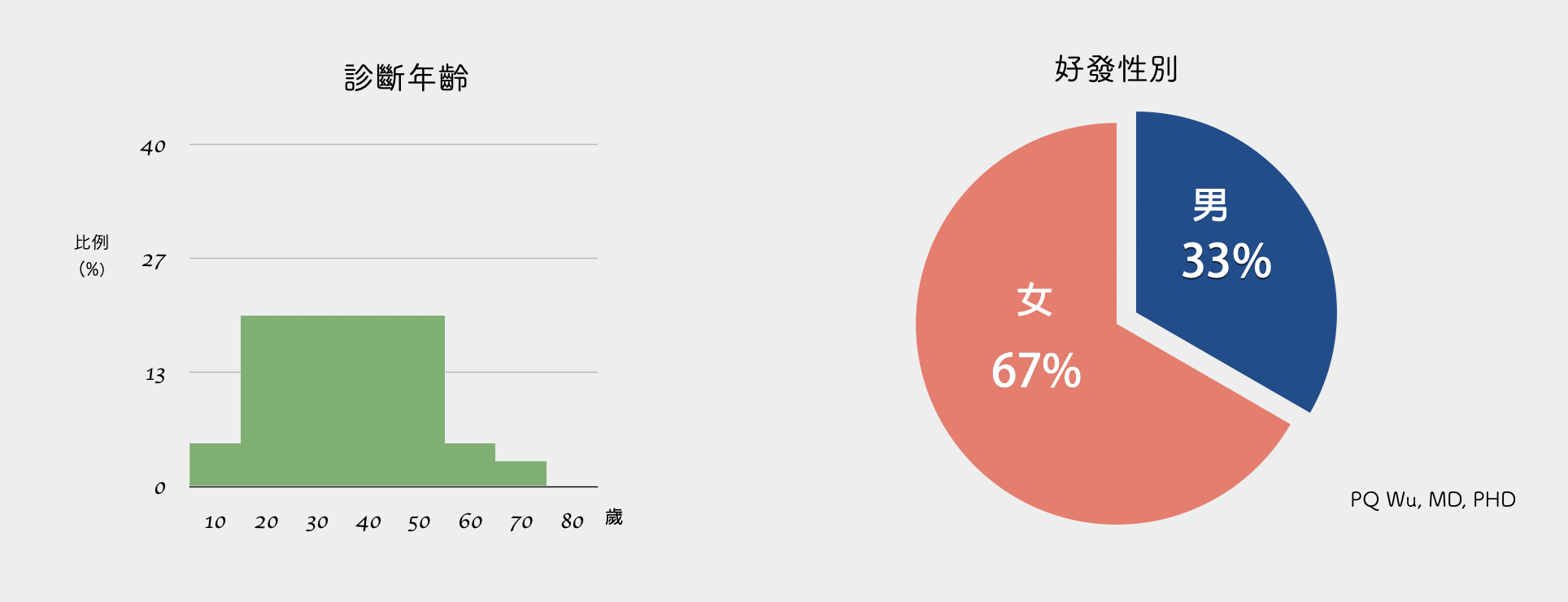
Gender and age
Fibroid tumors are more likely to occur in women, with about two to three times more than in men. If fibroid tumors occur in the abdominal cavity, the patients are mostly young adults around 30 years old. However, if fibroid tumors occur in the limb, the patient's age is between 20 and 60 years old.
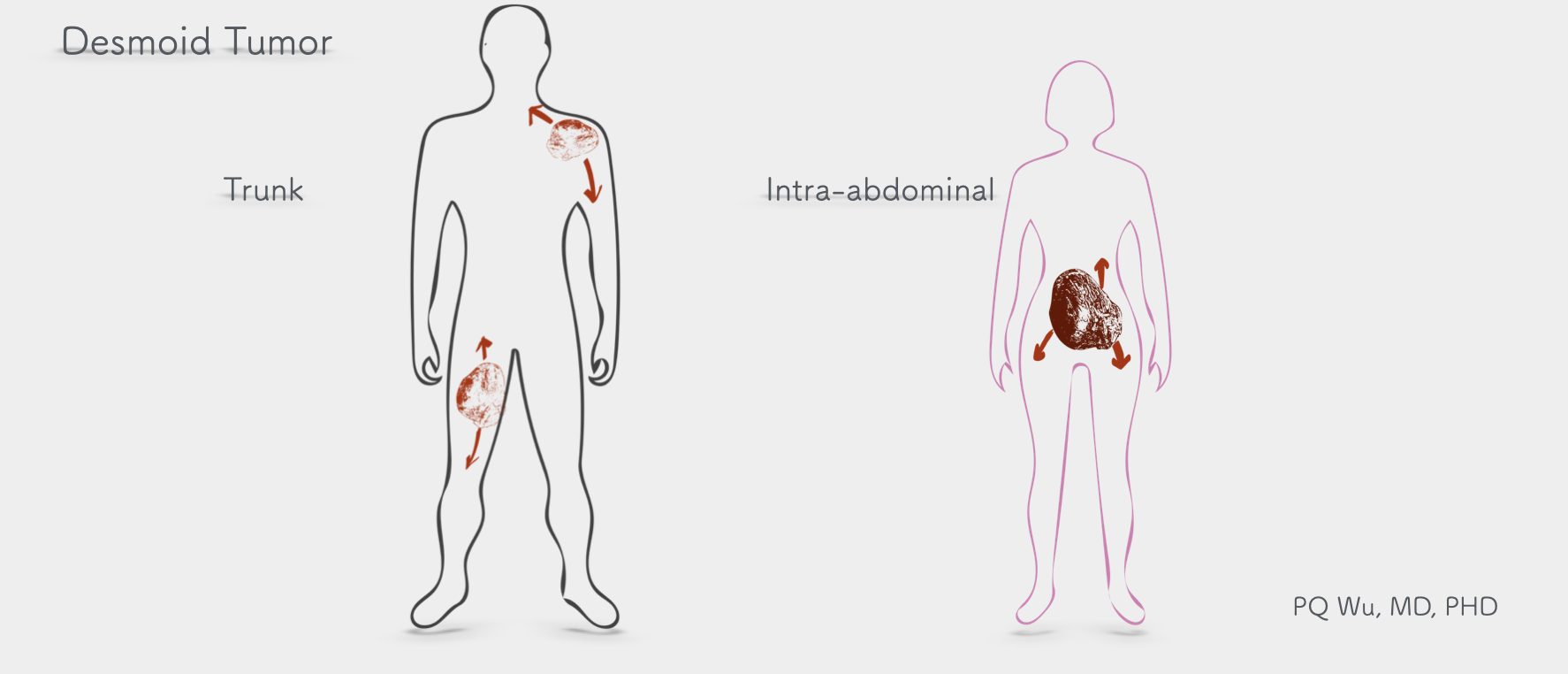
Tumor location
The most likely locations where fibroid tumors grow include shoulders and thighs. The tumor has the feature to invade along with the muscle, often causing serious effects on the patient's limb function. There is also a class of fibroid tumors that occur at the abdominal muscles (intra-abdominal desmoid tumors). The locations include the abdominal cavity, back, pelvis, and rear abdominal cavity. Tumors in these locations are usually quite large when discovered since they are asymptomatic and not easy to detect! In addition, about 2 percent of fibroid tumors are multiple and occur simultaneously in different locations in the body.
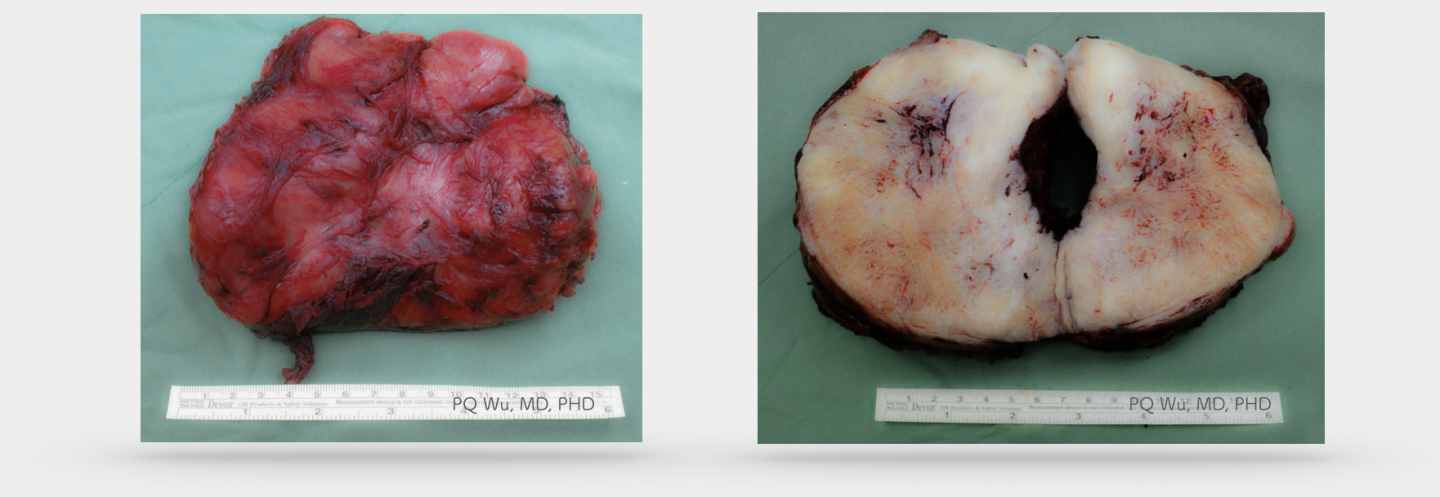
Pathology
A specimen of a fibroid tumor looks like a large ‘Dried scallops.' It is filled with a white, fibrous texture and very solid. So a fibroid tumor is quite hard (rock-like) under a touch. Under the microscope, the edges of fibroid tumors are often immersed in surrounding muscle tissue or tendons instead of having a complete margin that other tumors have. This feature is also the reason why the recurrence rate of fibroid tumor is quite high after surgery!
The cause of fibroid tumors
The cause of fibroid tumors is considerably related to genes. One of the key elements is the influence on the β-Catenin protein. So, before we dive into the cause, let's look at what function the β-Catenin protein has. In most cases, β-Catenin works with Cadherin to regulate cell-to-cell connections and interactions. However, to regulate the concentration of β-Catenin in cells, a group of complex proteins, including APC, axin, GSK3, and CK1, will metabolize β-Catenin to avoid its excessive concentrations within the cell. I have drawn the following diagram to facilitate your understanding.
After understanding the function of the β-Catenin protein, let's take a look at a fairly well-known pathway, the Wnt pathway. The canonical Wnt pathway is triggered in special physiological (embryonic development, self-renewal of stem cells in wound repair) or pathological (canceration) situations. When Wnt is attached to a receptor on the cell membrane, the disheveled protein is activated, and the metabolism of β-Catenin is inhibited. Because β-Catenin cannot be metabolized, the concentration of β-Catenin in cells increases significantly and enters the nucleus to interact with transcription factors, triggering a series of downstream reactions. You can see the figure below for a detailed mechanism.
Once we understand the β-Catenin and the Wnt pathway, we can explain the genetic problems that occur with fibroid tumors. There are two genetic mutations in fibroid tumors. The first is a mutation in the gene that produces the β-Catenin protein (CTNNB1, located on chromosome 3p22.1), resulting in an increased concentration of β-Catenin because of the excess structural rigidity of β-Catenin. This genetic mutation accounts for 85 percent of fibroid tumors.
The other 15 percent of fibroid tumors are associated with Familial Adenomatous Polyposis (FAP), known as Gardner's syndrome. According to a 2008 study, patients with a FAP are 10-20% more likely to have fibroid tumors, which is 852 times more likely than the general population. Mutations in the APC (Adenomatous polyposis coli) gene in patients is a reproductive mutation that is therefore inherited. Once the APC mutates, its function decreases, resulting in the inability of metabolizing of β-Catenin and generating in fibroid tumors. This type of fibroid tumor has three different characteristics compared to the CTNNB1 mutated fibroid tumors aforementioned: First, it occurs more in men. Second, the patients are younger. Third, it will be easier to appear in the abdominal cavity and pelvis.
*Seow-Choen F. The management of desmoids in patients with familial adenomatous polyposis (FAP). Acta Chir Iugosl 2008;55:83–7.
Fibroid tumors won’t have malignant transformation. However, some fibroid tumors are difficult to be distinguished from low-grade malignant fibrosarcomas in both imaging and pathology in the initial diagnosis. The low-grade fibrosarcomas, which are thought of as fibroid tumors, are sometimes determined after a few surgeries for recurrence treatment.
Fibroid tumors do not cause lung metastasis.
In a 2011 study published in the Journal of Clinical Oncology(*), several key factors that affect the recurrence of fibroid tumors are reported. In a looser univariate analysis study, the poor prognosis would correlate to the age of patients under 37, with tumor size greater than 7 centimeters, and with microscopic residual tumor location outside the abdominal cavity. However, in the rigid multivariate analysis, only the residual tumor size and locations are correlated to prognosis.
*Prognostic Factors Influencing Progression-Free Survival Determined From a Series of Sporadic Desmoid Tumors: A Wait-and-See Policy According to Tumor Presentation. J Clin Oncol. 2011;29(26):3553-3558.
There are several types of drug treatment for fibroid tumors:
1. Hormone (estrogen) therapy. In 1986, scientists first discovered that fibroid tumors grew more rapidly in pregnant women (*). It is generally recognized that hormone is likely to be associated with the development of fibroid tumors. So, the medical community began to use the hormone to treat fibroid tumors. Based on past experiences, it has been found that patients who have used estrogen may have tumor size reduction. However, there is no direct scientific evidence. In 2006, a joint study published on Cancer by Chicago University and Emory University at Georgia on 40 patients with fibroid tumors outside the abdominal cavity demonstrated that all tumors showed Estrogen Receptor-β. Hence, it can be proved that many hormone treatments, including tamoxifen, selective estrogen receptor modulators (SERMs) and so on, have their theoretical basis. Unfortunately, although hormone therapy has some effect, only about 50 percent of patients can get the tumor under control.
2. NSAID. In the 1980s, Waddell WR, a surgeon at Denver, occasionally found that the use of NSAID in large intestine polyps treatment shrink the fibroid tumors in the patient (**). He published this discovery in the Journal of Surgical Oncology at that time, but the reasons for the effect were unclear. It was not until later studies recognize that NSAID (COX2) could activate platelet-derived growth factor receptors, influencing the aforementioned Wnt pathway and achieving the tumor suppression effect.
*The desmoid syndrome. New aspects in the cause, pathogenesis and treatment of the desmoid tumor. Am J Surg. 1986 Feb;151(2):230-7.
** Indomethacin and ascorbate inhibit desmoid tumors. J Surg Oncol. 1980;15(1):85-90.
Radiation therapy for fibroid tumors can be used as 'standalone' or ‘complement surgery.' According to a study published in Cancer in 2000 (*), about 78% of fibroid tumors can be locally 'controlled' (not cured) by radiation therapy. Although there are good results, since patients are generally younger, clinicians would have concerns about the following problems by radiation. So, sometimes they would be more conservative to the use of radiation therapy!
*Surgery versus radiation therapy for patients with aggressive fibromatosis or desmoid tumors: a comparative review of 22 articles. Cancer 2000.