Before the 1980s, soft tissue sarcoma is deemed as an amputation-oriented disease. Most patients will need amputations or disarticulation surgery to save their lives, causing significant physical and mental damages. Fortunately, in the past decade, with the continuous improvement of chemical drugs, radiology, radiotherapy, surgery, and the advance of local cryotherapy technology, the amputation rate of patients has been less than five percent in the Therapeutical and Research Center of Musculoskeletal Tumor in Taipei Veterans General Hospital. Most patients can receive limb retention surgery.
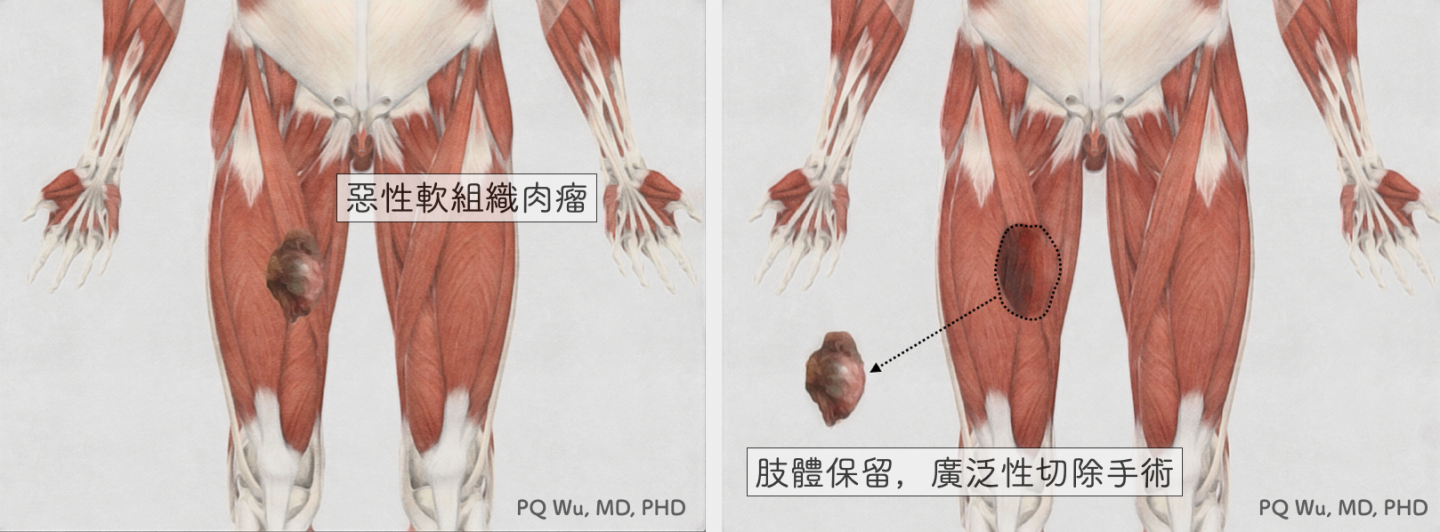
As the name implies, Limb salvage is to remove only the tumor from the patient rather than remove the patient's limb entirely. Almost all patients and physicians want to conduct limb salvage for patients with malignant osteosarcoma. Still, the key determinator is the degree of their tumor invasion and the extent of their disease. Generally, if the tumor is quite large and has invaded the entire important limb nerves and blood vessels, retaining the dilapidated limb will bring greater distress.
It will require the physician to take about five to ten times more surgery time and more concentration to perform limb salvage surgery than amputation. It takes a considerable amount of time to carefully remove the tumor, avoid damage to important nerve vessels, and spend much more effort reconstructing the limb. As a result, physicians who are able to perform this surgery are required to undergo a considerable amount of time for double specialist training. Also, since in Taiwan, the amount of patients with soft tissue sarcoma is small and most of them concentrate in some hospitals, the physicians specializing in osteosarcoma are scarce. (Note: Although hard as it is, it's worth it to see the patients gradually recover from surgery!)
The missions of limb salvage surgery are two:
First: Remove tumor (Wide Excision)
Second: Restore limb function (Limb Reconstruction)
Both are indispensable and are must-to-have. If the tumor is not removed completely, even if the postoperative limb function is excellent, after a few months, the tumor will recur. If the tumor is cleaned up thoroughly, but the limb reconstruction is incorrect, the patient is still unable to walk (or move the upper limb), it’d be better to conduct a direct amputation.
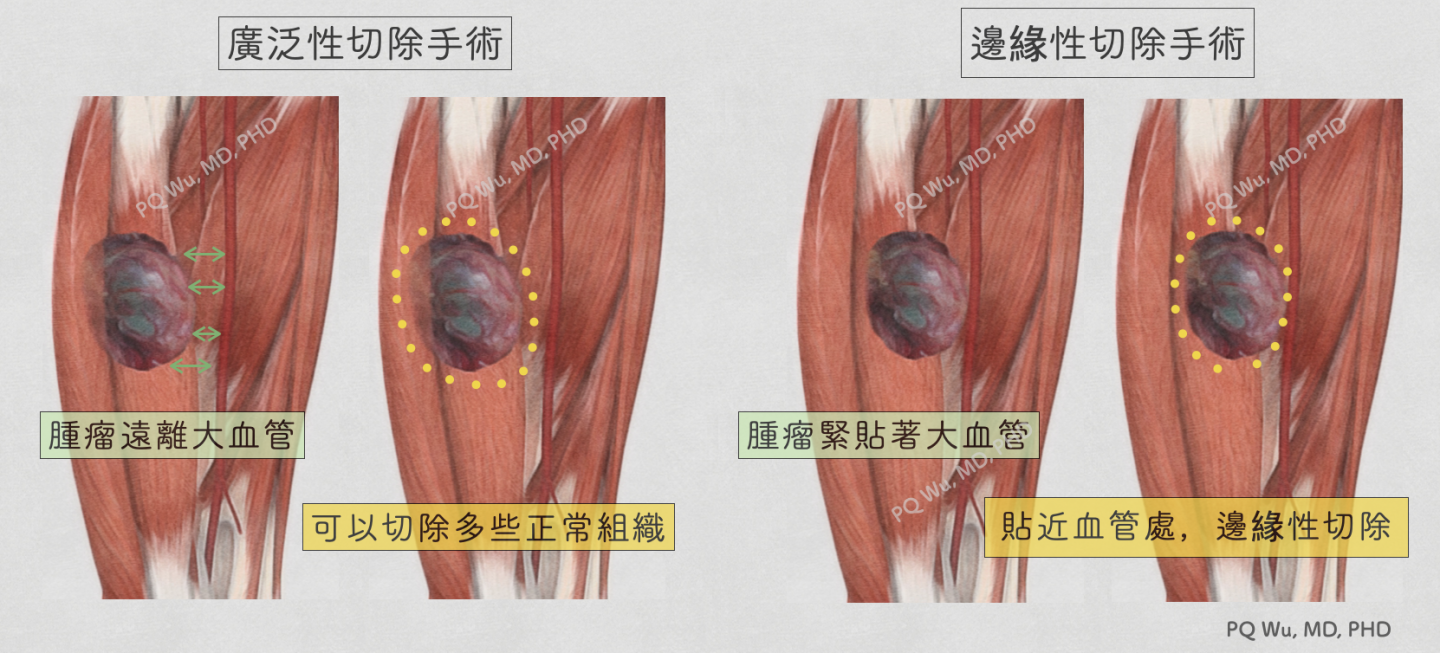
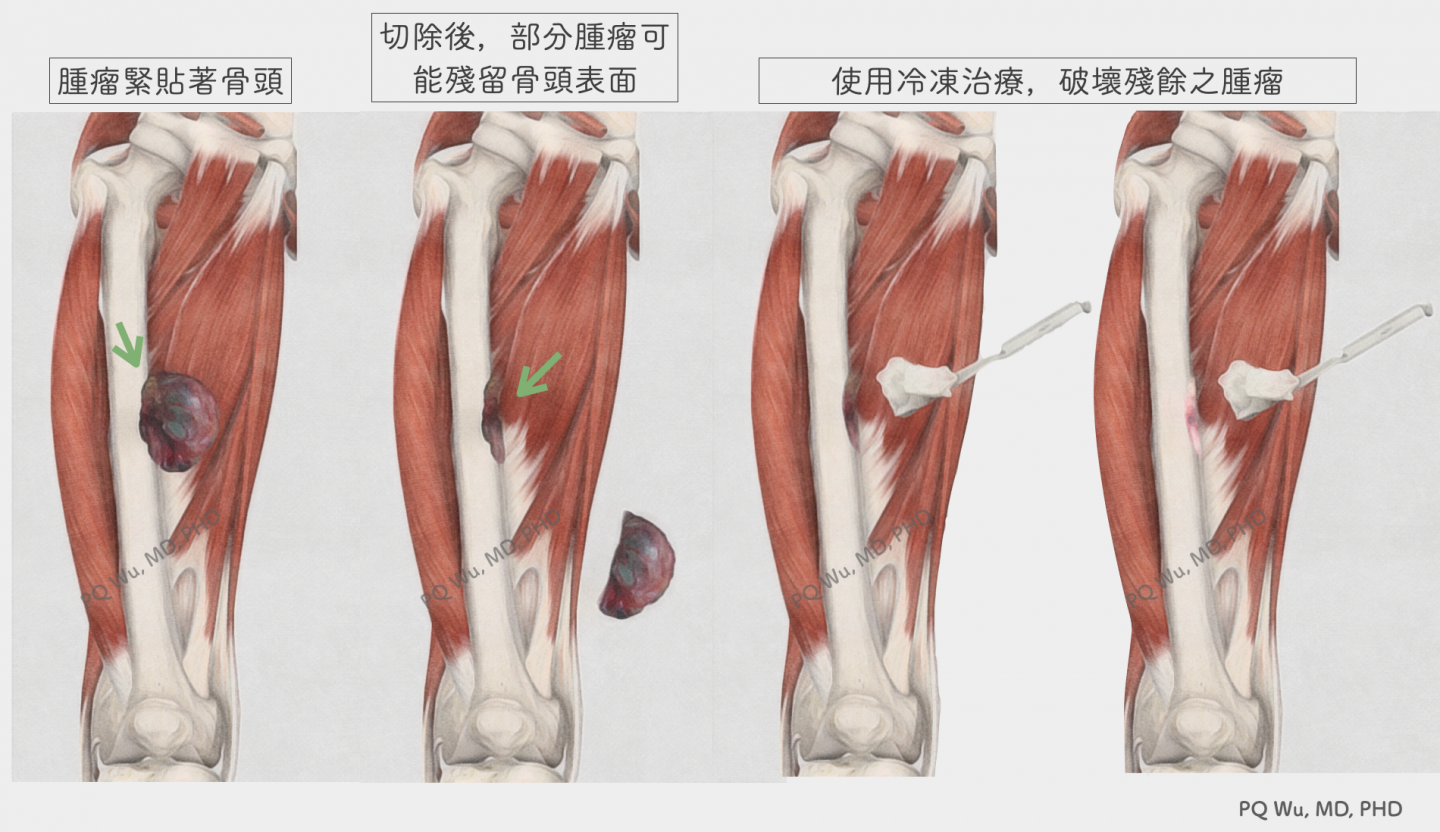
The greatest advantage of "marginal resection" is that it retains more normal tissue and hopes to enable patients to achieve better post-surgical functional recovery. Yet, the risk that we may take is a 'residual tumor'. In general, the residual tumors are mostly invisible. The reason for the residual may be that the surgery is not wide enough because we want to preserve important normal tissue, or it may be that a small number of cells from the tumor itself grow sparkling around the original tumor, i.e., satellite lesions. Therefore, to reduce the occurrence of these situations, we apply cryotherapy technology to destroy the potentially residual tumors after tumor removal in the Therapeutical and Research Center of Musculoskeletal Tumor in Taipei Veterans General Hospital. Through the implementation of this technology, the chance of tumor recurrence can be greatly reduced theoretically.
Generally speaking, we won’t conduct intralesional curettage to malignant bone tumors since it greatly increases the chance of tumor recurrence. So, unless for special concerns, this practice is not considered.
Although the proportion of amputations is currently quite low, the need for amputations is still unavoidable in some cases.
1. The range of tumor invasion is too large, and the tumor invades important blood vessels and nerves. If we perform wide excision, the blood vessels and nerves will inevitably be damaged, and functionless limbs will be left. It won’t be better if the patient receives amputation and wear the prosthetic to function afterward.
2. The tumor grows in special and rare anatomical areas, such as ankles or feet, causing the difficulty of reconstruction after tumor removal.
3. The tumor recurs after surgery, and the recurred tumor has no obvious boundary with the normal tissue and nerves or blood vessels.
Fortunately, these three conditions are not common, and most patients can take limb salvage surgery