Alveolar soft part sarcoma, or ASPS, is a rather rare and highly malignant soft tissue sarcoma. It was first discovered and named in 1952 by Dr. Christopherson and his colleagues. The biggest feature of alveolar soft part sarcoma is that local tumors grow quite slowly and are often discovered months or years after it becomes ill. However, although it grows slowly at the local regions, it has a considerable strong ability to metastasize distally. As a result, about 60% of patients have had lung metastasis at the time of diagnosis, and it influences considerably on prognosis.
Chinese:肺泡狀軟組織肉瘤 English: Alveolar Soft Part Sarcoma, ASPS
Most patients do not have pain. Most of the lesions are discovered only after the patients feel a swollen or noticeable lump at the lesions.
Alveolar soft part sarcoma is a rare malignant soft tissue sarcoma, accounting for about 0.5% to 1% of all malignant soft tissue sarcoma. Since it is quite rare, there are currently only 14 cases at the Therapeutical and Research Center of Musculoskeletal Tumor in Taipei Veterans General Hospital.
Alveolar soft part sarcoma is more likely to occur in women, taking about 60 percent. Most of the cases occur in young people between the ages of 15 and 35.
A 20-year-old female with alveolar soft part sarcoma on the back of her calf.

Alveolar soft part sarcoma invades local veins and combines vascular obstruction.
Most alveolar soft part sarcomas occur in the deep muscles of the limb, most commonly the thighs and torso. However, if in children, it often occurs in other more specific positions such as head, neck, eye frame, or tongue.
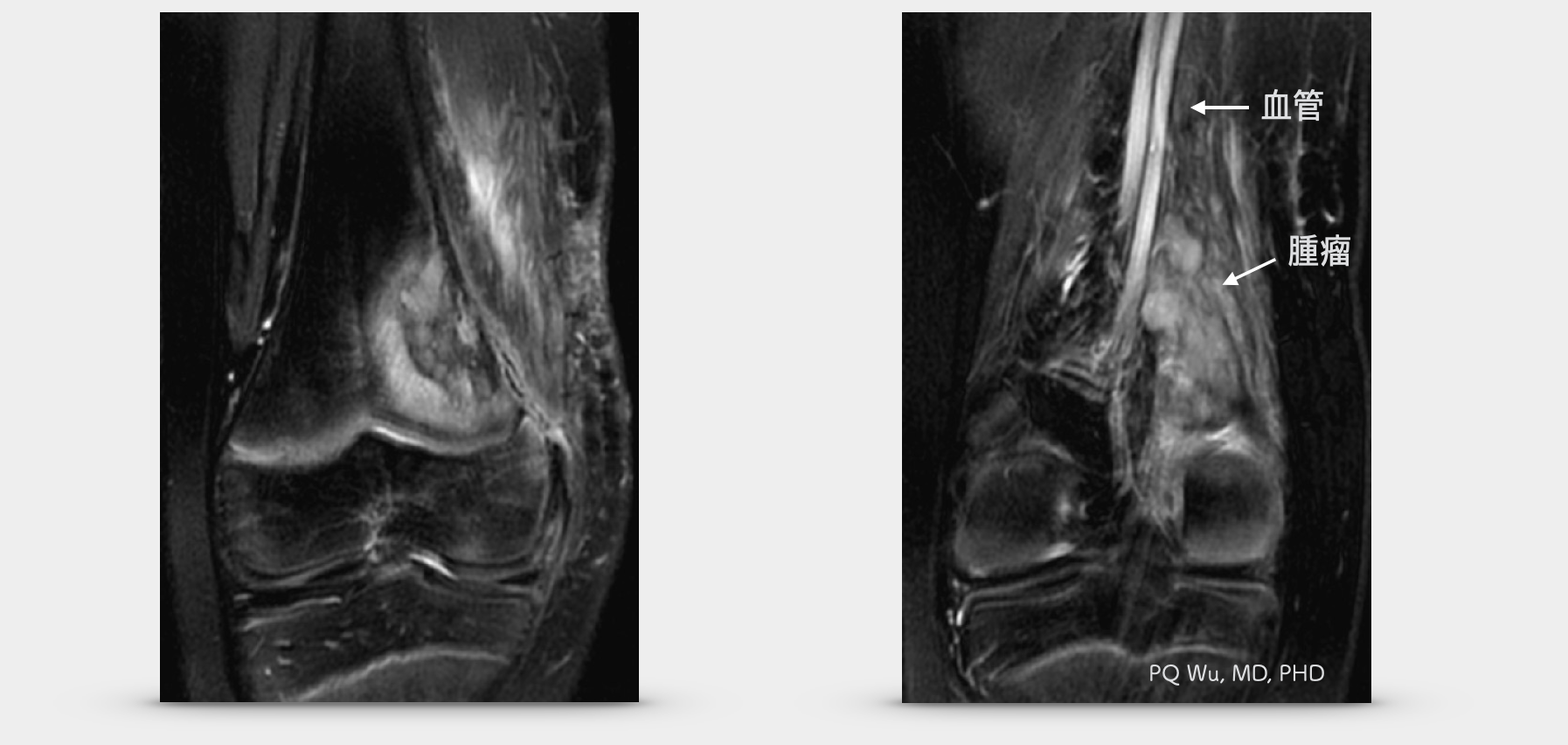
Figure above: 11-year-old male with distal alveolar soft part sarcoma in his thigh and the tumor invaded to the distal femur.
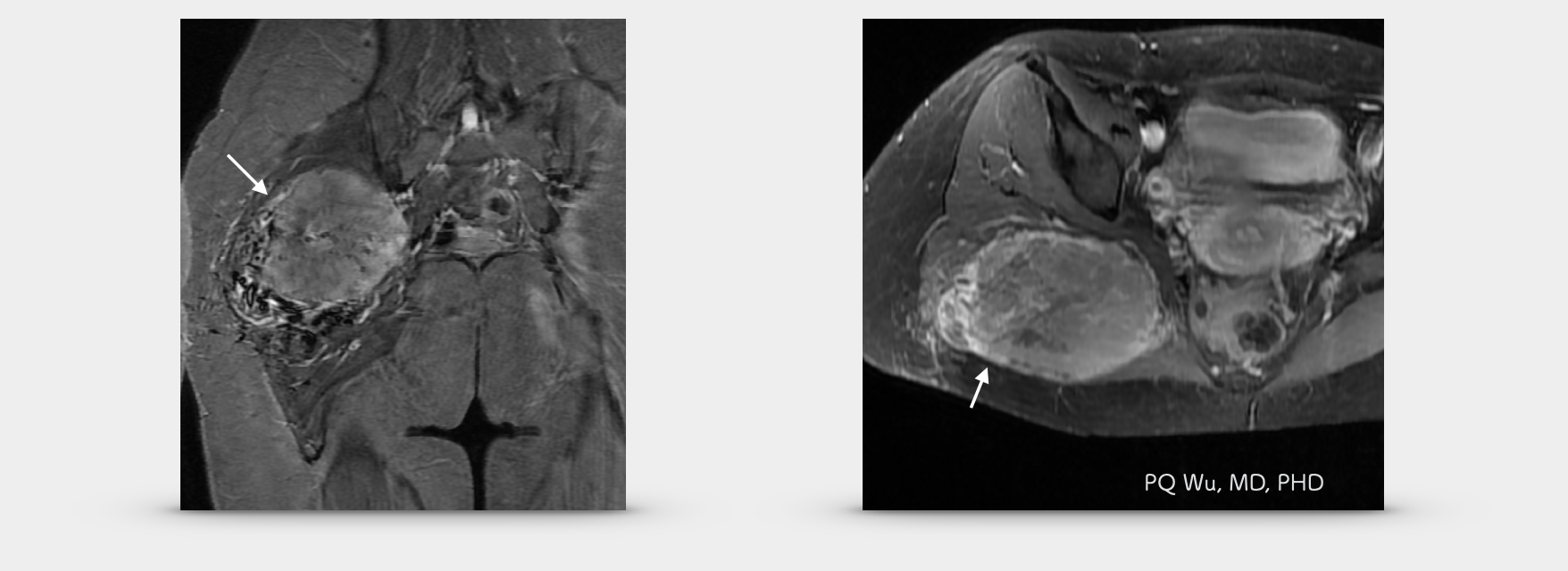
Figure above: 23-year-old female with alveolar soft part sarcoma at her hip.
Under X-ray, alveolar soft part sarcoma sometimes reveals calcification, yet it cannot be used for definitive diagnosis. MRI is relatively important for diagnosing alveolar soft part sarcoma. Under MRI imaging, alveolar soft part sarcoma exhibits fairly abundant blood supplies (highly vascularized). Also, both T1 and T2 will show hyperintense signals. This is a considerable difference between alveolar soft part sarcoma and other malignant soft tissue tumors.
However, it is quite troublesome that such abundant blood flows are quite similar to the features of hemangioma or arteriovenous malformation, AVM. Half of the alveolar soft part sarcoma was treated as benign vascular lesions, as reported in the literature. We also experienced such regret in our treatment for the alveolar soft part sarcoma patients at the Therapeutical and Research Center of Musculoskeletal Tumor in Taipei Veterans General Hospital!
Therefore, when we suspect that the patient has a hemangioma, it is better and safer to arrange an MRI or ultrasound examination to ensure that the tumor has no soft tissue component so that we can eliminate the likelihood of having an alveolar soft part sarcoma!
(Dr. Wu: In fact, this is quite difficult for doctors in Taiwan because the occurrence ratio of hemangioma and alveolar soft part sarcoma differ too much. Hence, unless the physicians are really specialized in bone tumors, they generally do not think of this rare disease. Moreover, the general physicians are afraid of subjecting patients for MRI examinations since the National Health Insurance will not reimburse if the lesions are not found eventually, making it even harder!)
The source of tumor cells for alveolar soft part sarcoma is currently unknown. Generally, it’s thought to be caused by the transformation of muscle cells. In 2001, Dr. M Ladanyi, a pathologist at the Memorial Sloan-Ketttering Cancer Center in New York, decrypted the cause for alveolar soft part sarcoma formation. He found that the cause was the translocation between the X chromosome and the 17th pair of chromosomes in the human body (t(17)t (X:17) (p11; q25) translocation). Then, in June of the same year, in collaboration with Johns Hopkins Hospital, he found that the translocation generated an abnormal fusion gene (ASPL-TFE3 fusion gene) increased the expression of its downstream fusion protein (nuclear TFE3-expression) and cancerized it.
The alveolar soft part sarcoma is quite specific in the pathological biopsy. A large number of consistent, nested polygonal tumor cells are generally visible. These groups of tumor cells are separated by many fibers and micro vessels. Since it looks like alveoli in the lungs, it is named 'alveolar' soft part sarcoma. The mitosis of the tumor cells is not obvious, and many tumor cell necrosis can be discovered. In a few less typical patients, we can conduct an immunohistochemistry test to identify the expression of nuclear TFE3. More, we can conduct a reverse transcription-PCR, RT-PCR to see if ASPL-TFE3 gene fusion exists.
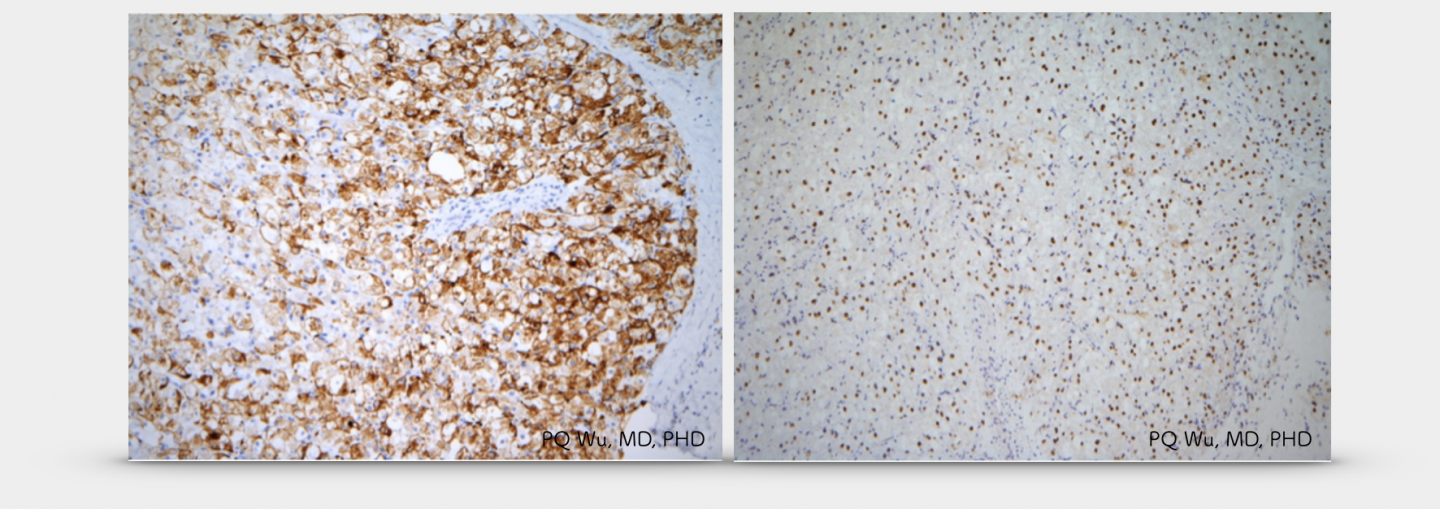
Figure above: Immunohistochemistry shows positive staining of TFE3 in the tumor nucleus
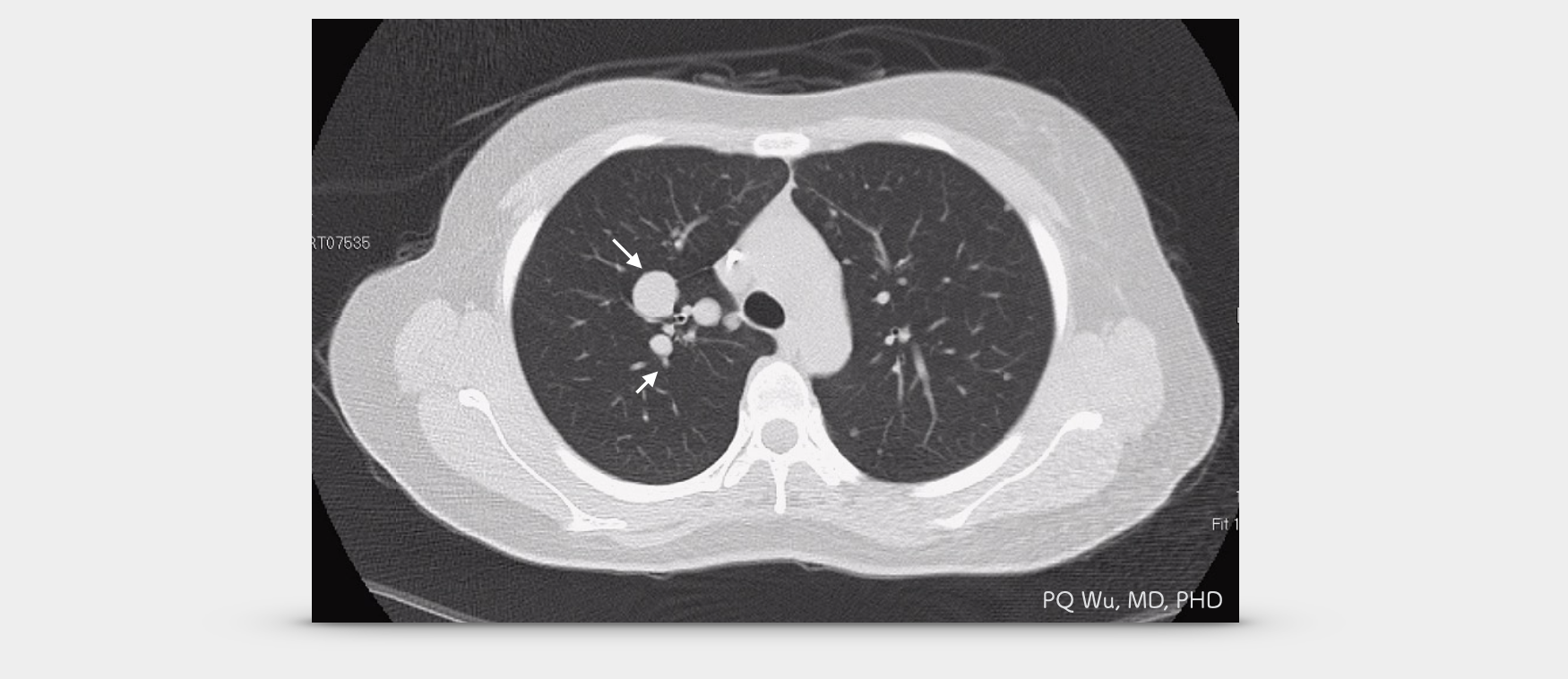
Compared to other malignant soft tissue sarcomas, alveolar soft part sarcoma has a very high metastatic potential. According to many literature reports, about 60% of patients will have metastasis, 25% of patients will be discovered the metastasized lesions when diagnosed with alveolar soft part sarcoma. The most common metastasis location is the lungs, followed by lymph nodes, bones, and the brain. Among them, brain metastasis is a very special characteristic of the alveolar soft part sarcoma. It takes about 30% of patients, and the incidence is more than three times as many as other malignant soft tissue sarcomas. Therefore, when a patient has neurological symptoms, the physician must consider the possibility of brain metastasis.
According to a 2010 report published in Annals of Surgical Oncology by Milan's Istituto Nazionale Tumori in Milan, an alveolar soft part tumor has 68.7% of the average five-year survival rate and 53.4% average 10-year survival rate. In another longer-term tracking report, the average two-year survival rate was 77%, the average five-year survival rate was 60%, the average 10-year survival rate was 38%, and the average 20-year survival rate was 15%.
According to numerous literature reports, the alveolar soft part sarcoma does not respond well to chemotherapy (resistant to conventional chemotherapy). Hence, a wide excision is important. If the tumor cannot be removed completely by surgery, post-surgical radiotherapy is required. However, as mentioned earlier, the alveolar soft part sarcoma is a rather easily metastatic sarcoma; therefore, surgery alone is not enough, and since the tumor is not very responsive to chemotherapy, the use of targeted therapy to treat alveolar soft part sarcoma has been started in recent years.
One well-known targeted therapeutic is Sunitinib, which is commonly used in renal cell carcinoma and gastrointestinal stromal tumor, GST, treatments. Because alveolar soft part sarcoma is rare, there is currently no large-scale study of using Sunitinib for its treatment. According to a 2010 study in Milan, Sunitinib was used in nine alveolar soft part sarcoma patients. After an average of 14 months of follow-up, five of the patients were found to have partial tumor reduction, three have stable courses, and only one of them with increased severity of the disease. However, because the tracking time is not long enough, it is still not strong clinical evidence.
Alveolar soft part sarcoma is a difficult opponent for physicians and patients. Prior to diagnosis, incorrect judgments were often made because of the rarity of the disease and the similarity of its imaging performance with hemangioma. After a correct diagnosis, distal metastasis often occurs, and its response to chemotherapy drugs is poor. As a result, it can only be surgically removed widely and be treated with targeted therapeutics. We hope that physicians and scientists can invent better weapons to deal with it in the next few years!